Can Wisdom Teeth Cause Migraines? Your Actionable Guide to Relief
- Caterina Rutter
- 1 hour ago
- 12 min read
Yes, your wisdom teeth can absolutely be a trigger for debilitating migraines. While connecting a tooth to a throbbing headache might seem odd, the link is surprisingly direct. When a wisdom tooth becomes impacted or infected, it can ignite a cascade of nerve irritation, muscle tension, and inflammation—a perfect storm for intense head pain. If you've suspected this connection, you're not just imagining it.
Understanding The Link Between Wisdom Teeth And Migraines
Have you ever had a pounding headache and a nagging suspicion it was tied to that ache in the back of your jaw? This is a common experience. Our third molars, or wisdom teeth, are notorious for arriving late, often into a jaw that has no room for them. This creates a chain reaction of problems that can travel far beyond your mouth.
An impacted wisdom tooth isn't just a simple toothache. Think of it as a hidden stressor, a constant source of low-grade irritation that can lower your body's threshold for a migraine attack.
When a wisdom tooth gets stuck, or "impacted," it pushes against neighboring teeth and, more critically, can aggravate the intricate web of nerves running through your face and jaw. The pressure doesn't just stay put; it can set off what's known as referred pain.
How Dental Pressure Becomes Head Pain
Referred pain is like a faulty electrical circuit. The problem might be a short in a wire behind one wall (your impacted tooth), but the light that flickers is across the room (the migraine pain you feel in your temple or behind your eye). Your brain receives a strong pain signal but misinterprets its origin.
This scenario is more common than you might think. Wisdom teeth typically emerge between ages 17 and 25, a time when many people already experience headaches. When these molars get impacted—meaning there isn’t enough space for them to erupt properly—they create pressure that can either trigger new migraines or worsen existing ones. This affects an estimated 90% of people at some point, making it a widespread issue. You can learn more about the connection between wisdom teeth and headaches on drbobbychhoker.com.au.
It's not just about direct nerve pressure. Several factors often work together:
Muscle Strain: When an emerging wisdom tooth disrupts your bite, your jaw muscles must work harder to compensate. This constant effort leads to tension headaches, which can easily escalate into a full-blown migraine.
TMJ Stress: This muscle strain puts significant stress on your temporomandibular joint (TMJ), the hinge connecting your jaw to your skull. TMJ dysfunction is a known trigger for severe headaches and facial pain.
Inflammation: A partially erupted or infected wisdom tooth can release inflammatory chemicals into your system. This increases your body's overall pain sensitivity, making you more vulnerable to migraines.
Actionable Insight: Instead of viewing wisdom teeth as just a dental issue, see them as a potential neurological trigger. The persistent, low-grade stress they place on your nerves, muscles, and joints can be the final push that turns a bad headache into a migraine. Recognizing this connection is the first practical step toward seeking the right diagnosis and finally breaking the pain cycle.
How a Tooth Problem Can Turn Into a Splitting Headache
To understand how a jaw problem can spark a debilitating migraine, you need to know about the head’s master nerve: the trigeminal nerve. Think of it as a massive electrical cable with branches running to your eyes, cheeks, and jaw. When a wisdom tooth is impacted or infected, it creates a persistent short circuit, sending chaotic pain signals up that cable straight to your brain.
This is a classic example of referred pain. Your brain receives the distress signal from the trigeminal nerve but gets confused about its origin. The wiring is so complex that a problem deep in your jawbone can manifest as pain behind your eye, in your temple, or across your forehead. It’s the body's version of a crossed wire.
This explains why many people are surprised to learn their recurring headaches are a dental issue. The problem doesn't always present as a "toothache"—sometimes, the only symptom is the head pain itself.
The map below illustrates this journey from an impacted wisdom tooth to nerve irritation, and finally, to a full-blown migraine.
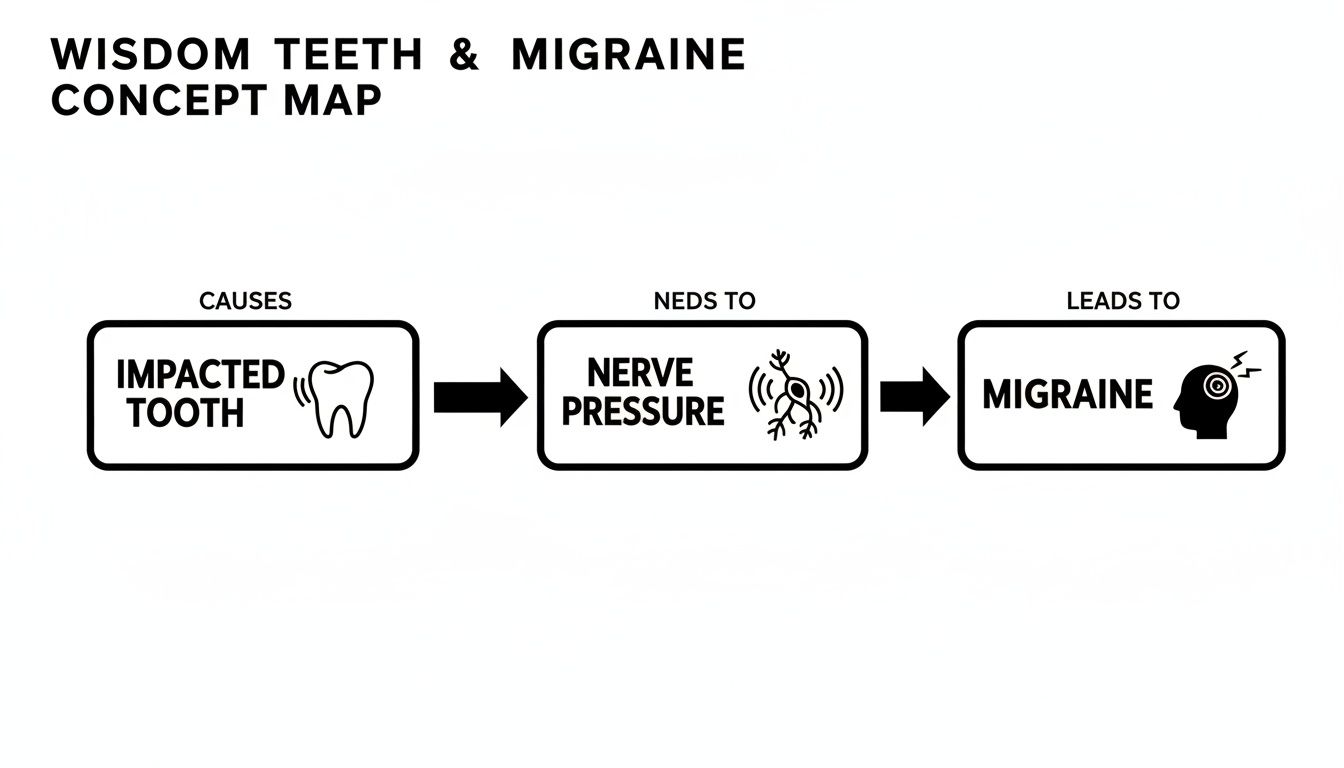
As you can see, a small, localized dental issue can easily escalate, firing pain signals along shared neural pathways and lighting up your entire head.
The Pathways From Your Jaw To Your Head
While direct nerve irritation is a huge factor, it's not the only way wisdom teeth can cause head pain. A few different things can happen simultaneously to create the perfect storm for a headache.
Direct Nerve Pressure: The most straightforward cause. An impacted wisdom tooth physically presses on the trigeminal nerve or its branches, creating constant irritation.
Chronic Muscle Strain: When a rogue tooth throws off your bite, your jaw muscles must work overtime, leading to fatigue and tension that creeps upward.
Inflammation and Infection: A partially erupted wisdom tooth is a magnet for bacteria. An infection can release inflammatory chemicals that make your entire system more sensitive to pain.
Unpacking Muscle Strain and TMJ Dysfunction
When a wisdom tooth grows sideways or lacks space, it can push other teeth out of alignment. This subtly changes your bite, forcing your jaw muscles into an awkward position every time you talk or chew. That constant, low-level strain creates deep muscle fatigue and painful knots—a classic trigger for tension headaches.
Over time, this muscle imbalance puts immense stress on your temporomandibular joints (TMJ), the delicate hinges in front of your ears. TMJ dysfunction is a notorious cause of migraine-like headaches, earaches, and facial pain. The link is so strong that many headache treatment plans start by addressing jaw tension. If this sounds familiar, it's worth learning how to treat TMJ at home for jaw pain relief.
Actionable Insight: Your body is a connected system. Strain in your jaw muscles doesn't stay in your jaw. It travels up through the muscles and nerves of your face and scalp, often culminating in a throbbing headache that feels miles away from your mouth. Pay attention to how your jaw feels in the morning—it's a key diagnostic clue.
The Role of Sinus Pressure and Inflammation
Another culprit, especially with upper wisdom teeth, is your sinuses. The roots of your top molars are located just below your maxillary sinus cavity. If an upper wisdom tooth becomes impacted or infected, the inflammation can swell and press against the sinus floor.
This creates a sensation nearly identical to a sinus headache, with pressure and pain behind your cheeks and eyes. You might be dealing with a double whammy: referred pain from the nerve and direct pressure on your sinuses.
Whether it’s through nerve pressure, muscle strain, or sinus inflammation, a problem wisdom tooth puts your body on chronic alert. This constant background noise lowers your migraine threshold. Suddenly, triggers you could normally handle—like stress or a sleepless night—are enough to push you into a full-blown migraine attack.
Identifying The Warning Signs And Symptoms
How can you tell if that pounding in your head is just another migraine or if your wisdom teeth are the root cause? The key is to look for clues that connect your head pain to what’s happening in your mouth. Knowing these specific red flags will help you have a more productive conversation with your dentist.
Moving beyond guesswork means knowing what to look for. A classic migraine might be set off by bright lights or stress, but a headache from a wisdom tooth problem often follows a different script. It frequently starts as a dull, nagging ache in your jaw that creeps upward.

Beyond The Headache Itself
When a wisdom tooth is the culprit, the headache rarely arrives alone. It usually brings other symptoms centered around your jaw, gums, and even your ears. These are the tell-tale signs that the root cause is dental.
Actionable Checklist: Symptoms to Monitor
Jaw Stiffness or Soreness: Do you wake up with a sore jaw? Does it feel tight or difficult to open your mouth fully? Check this box if yes.
Clicking or Popping Sounds: Listen for noises when you chew, yawn, or talk. These sounds can mean your jaw joint (TMJ) is under stress.
Unexplained Earaches: A deep, dull ache in or around your ear without signs of a cold or infection is often referred pain from an impacted wisdom tooth.
Visible Swelling: Look in the mirror at the very back of your mouth. Are the gums swollen, red, or tender? This is a clear signal something is wrong.
These symptoms can be subtle at first, building so slowly that you might dismiss them. But when they occur alongside your headaches, it’s a strong indicator that your teeth are involved.
Migraine Or Wisdom Tooth Headache Symptoms
While pressure from a wisdom tooth can trigger a full-blown migraine, the headache it causes on its own often feels slightly different. Use this table to compare symptoms and help identify the likely source of your pain.
Symptom | Classic Migraine Characteristics | Wisdom Tooth-Related Headache Characteristics |
|---|---|---|
Pain Location | Usually one-sided, often behind an eye or in the temple. | Often starts in the jaw or back of the head and radiates to the temple or forehead. |
Pain Type | Throbbing or pulsing. | A constant, dull, pressing ache that can become throbbing. |
Triggers | Often light, sound, stress, or certain foods. | Worsens with jaw movements like chewing, talking, or clenching. |
Associated Signs | Nausea, vomiting, and visual disturbances (aura). | Jaw pain, earache, gum swelling, and a bad taste in the mouth. |
Spotting the differences can be tricky, but that last row is often the most revealing. The additional symptoms provide the context needed to understand the true source of your pain.
Actionable Insight: The most telling sign is when your headache consistently intensifies with jaw activity. If chewing a tough piece of bread or clenching your teeth makes your head pound harder, that's a powerful clue that the problem originates in your jaw. Mentioning this specific trigger to your dentist can fast-track your diagnosis.
What To Expect During a Dental Diagnosis
Determining if your wisdom teeth are behind your headaches is not guesswork. It's a methodical process, and understanding the steps can reduce anxiety about your dental visit. It all starts with a targeted conversation.
You know your symptoms best, so we begin by listening. We’ll ask when the headaches started, where you feel the pain, and how it feels. More importantly, we'll connect the dots. Does the pain worsen when you chew? Is it more intense in the morning? These details help us form a working diagnosis.
The Hands-On Clinical Examination
After hearing your story, the next step is a thorough physical exam of your entire jaw system. Think of it as a detective gathering evidence at the scene—in this case, your recurring pain.
Here's what your dentist will actively look for:
Signs of Inflammation: We'll carefully inspect the gums around your wisdom teeth for redness, swelling, or tenderness—classic red flags for infection or irritation.
Checking for Impaction: We can often feel if a tooth is trapped under the gum or only partially erupted. An impacted tooth is a known troublemaker.
Testing Your Jaw Joints: We’ll ask you to open and close your mouth while we feel your jaw joints (TMJ). Any clicking, popping, or grinding can point to muscle strain that radiates pain upward.
This physical examination helps us confirm if our initial theory is correct.
The Power of Advanced Imaging
A physical exam tells us a lot, but the complete story is often hidden below the gums. That’s where imaging, like X-rays, is crucial. It provides a clear picture of your jawbone, tooth roots, and their positioning.
A panoramic X-ray is our go-to tool. It captures your entire mouth in one image, showing the exact position and angle of your wisdom teeth. We can immediately see if they are growing sideways, pushing against other teeth, or positioned too close to a major nerve. For more complex cases, a 3D Cone Beam CT (CBCT) scan provides a detailed 3D model of your jaw.
Actionable Insight: Imaging turns suspicion into a solid diagnosis. It eliminates guesswork by showing us precisely how a wisdom tooth might be causing nerve pressure, sinus issues, or crowding—all notorious headache triggers. This data allows us to create a targeted and effective treatment plan.
Armed with this clear picture, we can confidently determine if your wisdom teeth are the culprits. From there, we can map out a plan to get you relief. Our team is fully equipped to guide you through wisdom teeth removal in Tempe if it's the right solution to solve your pain.
Your Action Plan For Lasting Migraine Relief
Identifying wisdom teeth as a potential cause of your migraines is a huge step. But knowledge is only half the battle—the next step is taking action to find real, lasting relief. When the source of your pain is dental, a clear plan is the best way to navigate your treatment options and put the headaches behind you.

Often, the most effective solution is the most direct one: addressing the problem tooth. If your diagnosis confirms an impacted or troublesome wisdom tooth is the culprit, extraction is usually the recommended path.
The Definitive Solution: Wisdom Tooth Extraction
Think of it this way: removing a wisdom tooth that's causing nerve pressure, muscle strain, or chronic inflammation is like cutting power to a faulty alarm that won’t stop blaring. By eliminating the source of irritation, you stop the constant stream of pain signals being sent to your brain.
While the idea of surgery can be intimidating, wisdom tooth extraction is one of the most routine and predictable procedures in dentistry. It’s a straightforward outpatient procedure, meaning you’ll be resting at home the same day.
Actionable Insight: While wisdom teeth aren't always the direct cause of migraines, they are incredibly common triggers. They can provoke jaw clenching, nerve pressure, and TMJ strain, especially in people already prone to headaches. Post-extraction data often shows patients report significant headache relief within 3 to 7 days, with the problem frequently vanishing by the two-week mark. This rapid improvement is a strong indicator of the connection. Discover more insights about headache relief after extraction at theteethdoctors.com.
A smooth recovery is key to getting back on your feet quickly. For a detailed guide on aftercare, check out our article on how to recover from tooth extraction fast.
Exploring Non-Surgical Strategies
While extraction is often the ultimate fix, it isn't always the first or only option. In some cases, or as a temporary measure to manage pain before surgery, several non-surgical strategies can bring significant relief.
These approaches focus on managing symptoms and reducing strain on your jaw system.
Effective Non-Surgical Options:
Custom Night Guards: If your headaches are worst in the morning, you may be clenching or grinding your teeth at night due to your wisdom teeth affecting your bite. A professionally made night guard protects your teeth and eases the immense pressure on your jaw muscles and TMJ.
Targeted Physical Therapy: A physical therapist specializing in jaw function can help release deep muscle tension in your jaw, neck, and shoulders. Specific exercises can correct imbalances caused by dental issues, providing powerful headache relief.
Short-Term Medication: If an infection is brewing around a partially erupted wisdom tooth (pericoronitis), we may prescribe antibiotics or anti-inflammatory medications. This clears the immediate infection and reduces the swelling contributing to your pain, and is often a necessary first step before a safe extraction.
Creating Your Personalized Treatment Path
The right plan is always unique to you, depending on your wisdom teeth's position, symptom severity, and overall health. That’s why the first step is always a thorough evaluation.
During your consultation, we'll combine a detailed clinical exam with advanced imaging to get a clear picture of what’s happening. This allows us to map out a strategy that addresses the root cause of your pain.
Whether the best path forward is a straightforward extraction or a combination of non-surgical therapies, our goal is to give you a clear, step-by-step solution. You don't have to live in a debilitating cycle of migraines. A targeted plan can break that cycle for good.
Your Questions Answered: Wisdom Teeth & Migraines
When you're trying to determine if wisdom teeth are the real culprits behind your migraines, many questions arise. Here are practical answers to some of the most common ones.
Will My Migraines Disappear Right After My Wisdom Teeth Are Removed?
While many people experience a significant drop in headache frequency and severity, it's rarely an instant fix. Expect to feel initial relief within the first one to two weeks as post-surgical swelling and inflammation subside.
Remember, your body needs time to heal. If your jaw muscles and nerves have been under stress for months or years, they need a chance to reset. For some, it takes longer for migraine symptoms to resolve as that deep-seated irritation fades. The key is to look for steady, positive improvement during your recovery.
Can My Wisdom Teeth Cause Headaches if My Teeth Don't Hurt?
Yes, absolutely. This is a classic example of referred pain. Your trigeminal nerve is a massive sensory highway for your face, teeth, and jaw. An impacted wisdom tooth can quietly press on a branch of this nerve, sending a pain signal to your brain.
Your brain receives the signal but misinterprets its location. So, while the tooth itself feels fine, your brain registers the irritation as a pounding headache in your temple or behind your eye. The absence of a traditional toothache does not rule out a dental cause.
Actionable Insight: The absence of tooth pain doesn't mean your teeth are not the problem. If you have unexplained migraines accompanied by symptoms like a stiff jaw, earaches, or pain that worsens with chewing, a dental evaluation should be your immediate next step.
When Is the Best Time to Get Wisdom Teeth Looked At?
The best strategy is to be proactive. The ideal time for a first wisdom tooth evaluation is during the late teenage years, typically between 17 and 21 years old.
At this age, a panoramic X-ray can reveal how the teeth are developing and their likely eruption path. This gives us a clear picture of whether they are on track to become impacted or cause other problems. If they need to be removed, doing so before the roots are fully anchored in the jawbone generally leads to an easier procedure and a faster, smoother recovery—potentially saving you from years of future pain.
If you're in the Tempe area and suspect a link between your headaches and your wisdom teeth, you don't have to guess. The experienced team at Beautiful Dentistry can provide a clear diagnosis and a personalized plan to find real relief. Schedule your comprehensive evaluation today.



Comments