What is bone grafting for dental implants: Your guide to a stronger smile
- Caterina Rutter
- 7 days ago
- 14 min read
Let's cut right to it. Bone grafting for dental implants is a procedure that rebuilds your jawbone, creating a solid, reliable base for an implant. The best analogy is laying a foundation before building a house—if the ground isn't solid, the structure simply won't stand the test of time. Your key takeaway is that this common and successful procedure is often the first actionable step toward getting a permanent, confident smile.
Building the Foundation for a Lasting Smile
When you lose a tooth, the jawbone in that spot suddenly loses its job. Without the daily stimulation from chewing, the bone starts to shrink in a process called resorption. This natural response can leave the jaw too thin or soft to securely hold a dental implant, which needs a strong anchor to function just like a real tooth.
Understanding what bone grafting for dental implants is helps you take control of your treatment plan. The procedure involves placing special bone material into the jaw to signal your body to grow new, dense bone. This action builds up the necessary height and width for a successful implant.
Why Is a Strong Foundation Non-Negotiable?
A dental implant is a major investment in your oral health. To maximize that investment and achieve a 95% success rate or higher, the foundation must be perfect. Placing an implant in a weak jawbone is like setting a fence post in loose sand; it’s bound to wobble and eventually fail.
Here are the actionable benefits a bone graft provides:
Restores Bone Volume: It rebuilds bone lost from an extraction, gum disease, or injury, making an implant possible.
Provides Stability: It creates a dense anchor point for the titanium implant post, preventing movement.
Ensures Longevity: A solid foundation is the most critical factor for ensuring your implant lasts for decades.
The real purpose of a bone graft isn't just to fill a space. It's to kickstart your body’s own incredible ability to regenerate. The graft material acts as a scaffold, guiding your natural bone to grow and create a solid, integrated structure that's ready to support an implant.
This guide will walk you through everything you need to know about the bone grafting process. We'll cover why you might need one, the different types of grafts we use, and what to expect from start to finish. Our goal is to provide actionable insights so you feel fully informed and confident every step of the way.
Bone Grafting for Dental Implants At a Glance
To start, here’s a quick overview of what you need to know. Use this table to grasp the essentials before we dive deeper.
Concept | Brief Explanation |
|---|---|
What It Is | A procedure to add bone or a bone-like material to your jaw in an area that has lost volume or density. |
Primary Goal | To create a solid and stable foundation that can securely anchor a dental implant for long-term success. |
Who Needs It | Patients with insufficient jawbone height or width, often due to tooth loss, gum disease, or physical trauma. |
Success Rate | Extremely high. With success rates often exceeding 95%, it's a very reliable and predictable procedure. |
Now that you have the big picture, let's get into the specifics of how this all works.
Why a Strong Jawbone Is Crucial for Implant Success
Before we dive into what is bone grafting for dental implants, it helps to understand why your jawbone is so important in the first place. Think of it less like a static piece of your skeleton and more like a living, active foundation for your teeth. Every time you chew, bite, or talk, the roots of your teeth stimulate the jawbone, signaling it to stay strong and dense.
When you lose a tooth, that area of the jawbone loses its job. Without that daily workout, the bone begins to shrink and weaken—a process we call bone resorption.
This isn't a minor change. The loss can be surprisingly fast. In fact, you can lose up to 25% of your jawbone width in the first year alone after a tooth is gone. The actionable takeaway here is that waiting too long after losing a tooth can make the implant process more complex.
Common Causes of Jawbone Deterioration
While a missing tooth is a primary trigger for bone loss, it's not the only one. Be aware of these other common issues that can make a bone graft essential.
Here are the most frequent culprits we see:
Long-Term Tooth Loss: If a tooth has been gone for years, there's a very high chance significant bone has resorbed, often creating a noticeable dip in your jawline.
Advanced Gum Disease: A serious infection like periodontitis doesn't just attack your gums; it actively destroys the bone that holds your teeth in place.
Dental Trauma or Injury: A hard fall, a sports injury, or even a difficult tooth extraction can fracture or remove pieces of the surrounding bone socket.
Developmental Defects: Some people are simply born with less bone volume in certain areas of the jaw, making it too thin or short to support a standard implant.
Putting off treatment for these issues can lead to bigger problems, including a weaker bite and shifting of your remaining teeth. Acting sooner rather than later is always the best strategy.
Connecting Bone Health to Implant Success
Dental implants have an incredible success rate—often topping 98%—and that success all comes down to one key biological process: osseointegration. This is the magic that happens when the titanium implant post fuses directly with your living jawbone, creating an incredibly strong, stable bond.
But for osseointegration to occur, the implant needs something to fuse with. There must be enough healthy, high-quality bone to envelop the implant and anchor it securely. Trying to place an implant in a thin, weak jawbone is like planting a tree in a thimble of soil. It simply won't have the support to withstand the forces of chewing and will ultimately fail.
A bone graft isn't just an extra step; for many patients, it is the most critical part of the entire implant process. It rebuilds the foundation, ensuring your new implant has the solid support it needs to function just like a natural tooth for years to come.
Of course, your jawbone is part of a larger system, and overall bone health plays a role. Conditions like osteoporosis can impact bone density throughout your body. You can find more details in a guide to understanding bone health.
By taking the time to rebuild the site with a bone graft, we are creating the perfect environment for success, turning a compromised area into a solid foundation and securing your investment in a healthy, permanent smile.
Understanding the Four Main Types of Bone Grafts

Once we determine that a bone graft is the right move for you, the next step is deciding which type of material to use. This isn't a one-size-fits-all decision. The choice depends on your specific situation, how much bone we need to rebuild, and your overall health.
Think of it like laying the foundation for a house. You need the right materials to create a solid, stable base. In the same way, each type of bone graft material has its own unique properties and job to do in rebuilding your jaw.
The end goal is always the same: to create a sturdy scaffold that encourages your own body to grow new, healthy bone. Let’s walk through the four main types so you have a clear picture of your options and can participate confidently in your treatment planning.
Autografts: Your Own Bone
Often called the “gold standard,” an autograft uses a small piece of your own bone. It is typically harvested from another spot in your body—like your chin, the back of your jaw, or in some cases, the hip—and moved to where it's needed.
Because this bone comes directly from you, it’s packed with your own living cells and growth factors that signal your body to build new bone. This makes autografts incredibly effective at healing.
Key Advantage: Since it's your own tissue, there is absolutely zero risk of rejection or disease transmission.
Main Consideration: This approach requires a second surgical site, which can mean more initial discomfort and a slightly longer recovery.
For significant bone loss, the predictable and robust results often make it the best choice.
Allografts: Donated Human Bone
A very common and highly effective alternative is the allograft. This is bone from a human donor, sourced from a licensed and sterile tissue bank—similar to how other tissues and organs are donated.
This isn't just any bone. It goes through a strict screening and sterilization process that removes all living cells, eliminating any risk of disease transmission and ensuring the material is completely safe for you.
The biggest plus? An allograft avoids the need for a second surgical site, making the procedure simpler and your recovery a little easier. The donated bone acts as a perfect framework for your body to build upon, and over time, your own bone cells will completely replace the graft material.
Xenografts: Animal-Derived Bone
Another excellent option is a xenograft, which is bone sourced from an animal—usually a cow (bovine). Just like allografts, this material is put through a rigorous purification process that removes all organic material, leaving only the mineral structure behind.
This process ensures it’s perfectly safe and won’t be rejected by your body. The structure of bovine bone is remarkably similar to our own, making it an ideal scaffold for new bone to grow on.
Xenografts are especially popular because they break down, or resorb, very slowly. This provides a durable, long-lasting framework that helps hold the shape and volume of the jawbone for a long time—perfect for supporting a dental implant for years to come.
This slow-resorbing quality is also a huge benefit for procedures like sinus lifts, where maintaining space and structure is key.
Alloplasts: Synthetic Materials
Finally, we have alloplasts, which are entirely synthetic, lab-created materials. They are typically made from substances like calcium phosphate, which are biocompatible and mimic the natural minerals found in your own bone.
The main advantages here are an unlimited supply and a zero percent risk of disease transmission. These materials provide a clean, reliable scaffold that essentially gives your body's bone-building cells a blueprint to follow.
A Practical Comparison of Bone Graft Materials
Use this side-by-side comparison to quickly understand the key differences and help you discuss the options with your dentist.
Graft Type | Source | Key Advantage | Consideration |
|---|---|---|---|
Autograft | Your Own Body | Gold standard for regeneration; contains live cells. | Requires a second surgical site. |
Allograft | Human Donor | Avoids a second surgical site; excellent scaffold. | Relies on external tissue bank sourcing. |
Xenograft | Animal (Bovine) | Resorbs slowly, providing long-term stability. | Not your own tissue; derived from an animal source. |
Alloplast | Synthetic | Unlimited supply; zero risk of disease transmission. | Contains no natural growth factors. |
Ultimately, the best choice depends entirely on your unique clinical needs. We'll discuss the pros and cons of each as they relate to your specific case to make the right decision together.
The choice of material truly matters. Studies show just how reliable these procedures can be, with implant survival in autologous grafts at a 98.5% mean. Breaking it down further, block autografts show 98.9% survival, while particulate grafts hit a 100% success rate. These numbers underscore how choosing the right graft leads to incredibly predictable outcomes.
Your Bone Grafting and Implant Journey Step by Step
Thinking about a bone graft and dental implant can feel overwhelming, but seeing it as a well-planned journey makes it manageable. Each step is designed to build on the last, setting you up for a predictable outcome: a strong, permanent tooth.
Here is the complete roadmap of what you should expect, from your first visit to your final crown.
Step 1: Initial Consultation and 3D Imaging
Your journey begins with a discussion. We’ll talk about your goals, review your medical history, and answer every question you have. Most importantly, this is where we get a crystal-clear picture of your jawbone’s health.
We use an advanced 3D cone-beam computed tomography (CBCT) scanner to create a detailed, three-dimensional map of your jaw. This isn't your average dental X-ray. It gives us the power to measure the precise height, width, and density of your bone.
This scan provides the critical data we need. It tells us, without a doubt, if you can proceed directly to an implant or if we first need to build up a solid foundation with a graft.
Step 2: The Bone Grafting Procedure
If a bone graft is needed, that’s our next step. The procedure is done in our office with local anesthesia to ensure you’re completely comfortable. For anyone with dental anxiety, we offer sedation options to create a calm, stress-free experience.
During the procedure, your dentist will make a small incision in the gum to reach the underlying bone. Then, the graft material—whichever type we've selected together—is carefully placed in the exact area that needs more volume.
To finish, we often place a special protective membrane over the graft to shield it and guide healing. The gums are then comfortably repositioned and closed with a few small stitches.
Step 3: The Crucial Healing and Integration Phase
Once the graft is in place, the most important part begins: healing. This isn’t just about the gums closing up. Under the surface, your body is using the graft material as a scaffold to grow new, dense bone of its own. This process is called guided bone regeneration.
This healing period can take anywhere from four to nine months. Your action item here is patience. This phase is what creates the rock-solid foundation your implant needs to last a lifetime.
Think of this phase like allowing concrete to cure. You wouldn't want to rush it, because that would compromise the entire structure. Allowing the bone to fully mature is the single most important action you can take to guarantee the long-term success of your dental implant.
Step 4: Implant Placement Surgery
After confirming your jawbone has fully healed and is strong, it’s time to place the dental implant. Like the grafting procedure, this is done with local anesthesia. We'll precisely place a small titanium post—your new tooth root—into the strong, newly regenerated bone.
Once the implant is securely in position, another healing phase begins. For actionable steps on what to do before this type of appointment, check out our guide on how to prepare for oral surgery.
Step 5: Osseointegration and Your Final Tooth
Over the next few months, the implant and your jawbone will literally fuse together through a process called osseointegration. This creates an incredibly strong, stable bond, making the implant a permanent part of your anatomy.
When osseointegration is complete, we're on the home stretch. Here are the final action steps to restore your smile:
Abutment Placement: A small connector piece, called an abutment, is attached to the top of the implant.
Digital Impressions: We take precise digital scans of the abutment and your surrounding teeth—no more goopy impression trays.
Crown Fabrication: These scans are sent to our lab to design your final, custom-made crown, perfectly matched to your other teeth.
Final Placement: We securely attach the new crown to the abutment, completing your new tooth and giving you back a fully functional, beautiful smile.
Determining If You Are a Candidate for Bone Grafting
So, you’re considering dental implants but wondering if a bone graft is part of your treatment plan. Not every implant patient needs one, but figuring this out is a crucial first step.
The decision boils down to your jawbone's current state, your overall health, and your commitment to long-term oral care. The goal is simple: to give your future dental implant the strongest foundation possible for a lifetime of success.
An ideal candidate is someone in good general health who can heal well after a minor surgical procedure. This means that if you have any chronic conditions, like diabetes, they are well-managed. A healthy immune system is your best asset during healing.
Just as important is your dedication to excellent oral hygiene. A clean, healthy mouth is essential for the bone graft to heal properly. Your action plan should include consistent brushing, flossing, and keeping up with your regular dental visits.
Key Factors We Consider
While most people are great candidates, a few things require a closer look. Discuss these points with your dentist to create a plan that’s built for you.
Overall Health: Any conditions that might slow down healing need to be part of the conversation. We can coordinate with your physician to ensure you're ready for the procedure.
Oral Health: We must get any active gum disease or infections under control before placing a graft. A healthy mouth is non-negotiable for avoiding complications.
Smoking and Tobacco Use: Smoking restricts blood flow and can impede healing. Quitting or significantly cutting back will give your graft a much better chance at success.
Commitment to Aftercare: Following our post-op instructions is critical. This includes sticking to a soft diet for a short time and keeping the area clean as it heals.
The timeline below gives you a bird's-eye view of the entire journey, from that first chat and 3D scan all the way to placing the final implant after your graft has healed.
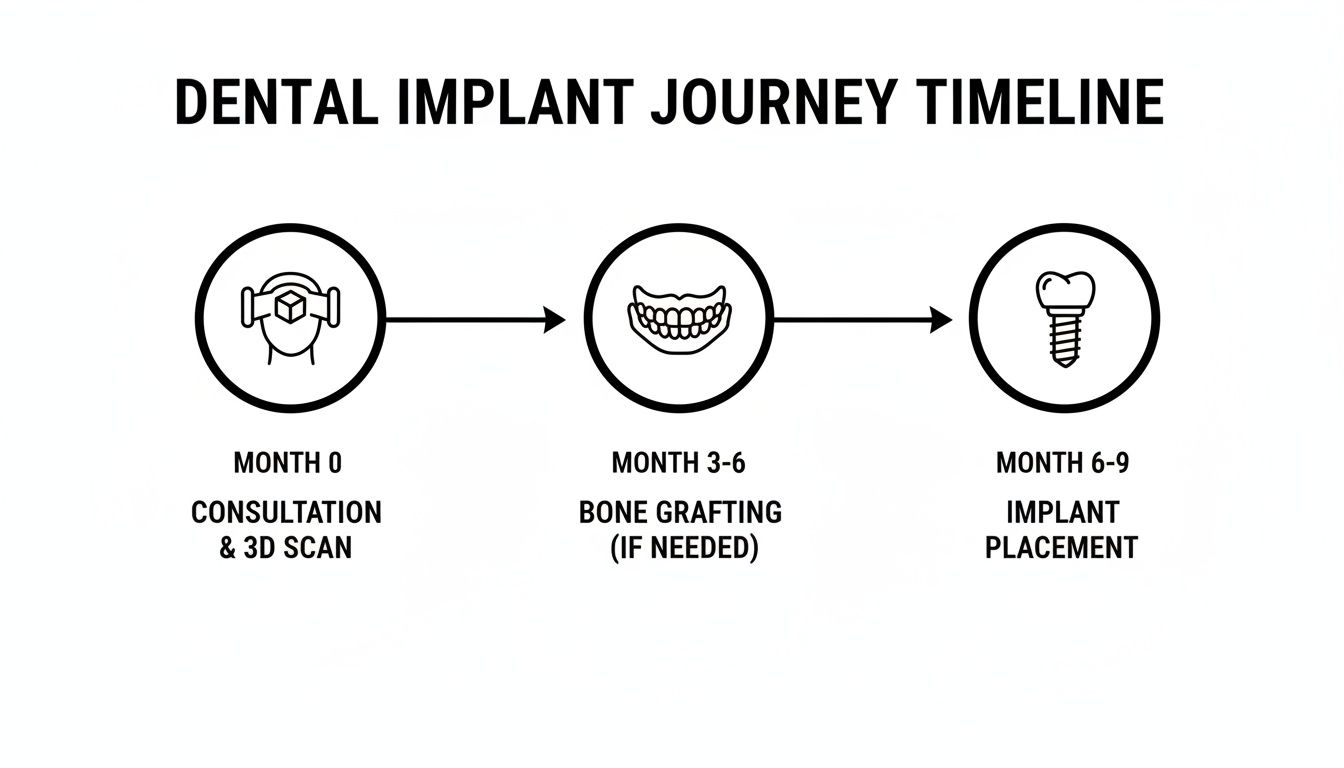
This visual roadmap shows how each step builds on the last, ensuring we get a stable and predictable outcome for your new tooth.
High Success Rates Pave the Way Forward
It's normal to hesitate about an extra step, but the results speak for themselves. Bone grafting is a highly reliable procedure, with studies showing success rates between 90% and 98%.
Even better, the implants placed in these healed sites do incredibly well, with a 97.2% survival rate. Your health habits play a huge role. For example, smoking can increase the risk of failure by 2.6 times, while simply maintaining great oral hygiene can slash that risk by 80%.
The most important thing to remember is that being a good candidate isn't about being perfect—it's about having a solid plan. By identifying and managing any potential risks together, we can create a clear path to success for almost anyone.
The only way to know for sure what your jaw needs is to have it professionally evaluated. Our advanced 3D imaging gives us an incredibly precise look at your bone structure, which removes all guesswork from your treatment plan.
To learn more, check out our guide on who is a good candidate for dental implants. Your initial consultation is the perfect opportunity to get clear, honest answers tailored specifically to you.
Your Bone Grafting Questions, Answered
It's one thing to understand the science, but another to know what to expect in practice. Feeling prepared is key to feeling confident. Here are direct answers to the practical questions we hear most often.
Is the Bone Grafting Procedure Painful?
No, the procedure itself is not painful. We use a very effective local anesthetic to completely numb the area before we start, so you won’t feel anything at the surgical site.
If you're nervous, we also offer several sedation options to help you feel deeply relaxed. Afterward, any discomfort is typically mild and easily managed with over-the-counter pain medication. We will provide you with a clear set of aftercare instructions to ensure your recovery is as comfortable and quick as possible.
How Much Does a Bone Graft for a Dental Implant Cost?
The cost depends on your individual situation. The two biggest factors are the amount of bone needed and the type of grafting material used. A small graft to fill an empty tooth socket will cost less than a more complex procedure to restore a larger area of the jaw.
We believe in full transparency. During your consultation, we will provide a detailed treatment plan that breaks down all costs—no surprises. Our team is also excellent at working with dental insurance and can help you maximize your benefits to manage the investment in your smile.
How Long Is the Recovery After a Bone Graft?
Think of recovery in two parts. First is the initial healing of the gums, which takes about one to two weeks. During this time, your main actions are to take it easy and stick to soft foods while any swelling subsides.
The second, more important part is bone integration. This is where your body builds new, strong bone around the graft. This process is crucial and takes anywhere from four to nine months. Patience during this phase is the best action you can take to ensure your jaw will be solid enough to support an implant for life.
The initial recovery is about the gums healing, but the full recovery is about the foundation solidifying. Rushing this crucial step would be like building a house on wet concrete; the long-term success depends on giving the bone the time it needs to mature.
Can I Get a Dental Implant Without a Bone Graft?
Yes, but only if your jawbone already has enough height, width, and density to securely hold an implant. We take the guesswork out of the equation by using advanced 3D imaging to get precise measurements of your bone.
If the scan shows the bone is too thin or soft, placing an implant would be like planting a tall tree in a very shallow pot—unstable from the start and destined to fail. A bone graft isn't an upsell; for many people, it's the single most important step to protect their investment and ensure their dental implant is successful for decades to come.
Ready to get a clear, personalized plan for your smile? At Beautiful Dentistry, we combine advanced technology with a compassionate approach to ensure your journey to a healthy, permanent tooth is a positive one. Schedule your $59 new patient consultation and exam today!



Comments