Understanding Your Dental Bone Graft Success Rate: An Actionable Guide
- Caterina Rutter
- Nov 10, 2025
- 11 min read
When you're told you need a dental bone graft, your first question is likely, "Will this actually work?" The answer is overwhelmingly positive: the dental bone graft success rate is consistently high, typically well over 95%.
However, that number isn't a guarantee. Your success depends on your health, your habits, and how well you follow post-operative instructions. Think of it like preparing the soil in a garden before planting a tree. A successful graft builds a strong, healthy foundation that your future dental implant needs to thrive for years. This guide provides the actionable insights you need to ensure the best possible outcome.
Why Dental Grafts Are So Successful

When a tooth is lost, the jawbone underneath it no longer gets the stimulation it needs from chewing and begins to shrink. This natural process, called resorption, can create a weak spot that can't support a future implant. A dental bone graft is a highly predictable procedure designed to rebuild that lost bone, creating a solid base for a dental implant.
This isn't an experimental procedure; it's a reliable cornerstone of modern dentistry. Studies consistently show that implant surgeries including a bone graft have a success rate between 95% and 98%. Considering millions of dental implants are placed annually in the U.S. alone—many requiring a graft—that statistic speaks volumes about its effectiveness.
What Does a "Successful" Graft Actually Look Like?
The true goal of a bone graft isn't just to fill a void; it's to trigger your own body to grow new, healthy bone. The graft material acts as a scaffold, providing a framework for your natural bone-forming cells to build upon.
Over the next few months, your body replaces that scaffold with your own living bone tissue in a process called osseointegration. A successful outcome means the new bone is strong and dense enough to securely anchor a dental implant for the long haul. This is what allows for advanced solutions to have a rock-solid foundation. You can see how this foundation is critical in our guide to All-on-X dental implants.
A dental bone graft doesn't just add volume; it triggers a natural biological response. Its success is measured by your body's ability to integrate the material and regenerate strong, living bone capable of supporting an implant for life.
Ultimately, the high dental bone graft success rate comes down to a powerful combination of advanced materials, precise surgical techniques, and your body’s incredible ability to heal.
Why a Bone Graft Is a Crucial First Step for Your Implant
A common question is, "Why can't I just get my implant now?" The answer gets to the heart of what makes an implant last a lifetime: the health of your jawbone. It’s easy to view a bone graft as an extra step, but it’s the most important investment you can make in the long-term success of your new tooth.
Think of your jawbone as the foundation of a house and the implant as a structural wall. You wouldn’t build on soft ground or a crumbling concrete slab. Placing a high-tech implant into a jawbone that’s too thin or soft is setting it up for failure. The graft is the essential repair that makes a secure, lifelong tooth replacement possible.
What Causes Bone Loss in the First Place?
Understanding what weakens this foundation helps you see why a graft is often necessary to achieve a high dental bone graft success rate.
Three main culprits are behind most jawbone loss:
Tooth Extraction: The moment a tooth is pulled, the bone loses its job. Without the daily stimulation from chewing, the body starts to reclaim those unused bone cells, causing the jaw ridge to shrink.
Gum Disease (Periodontitis): This destructive infection attacks the very bone supporting your teeth. As it progresses, it eats away at the jaw, leading to loose teeth and a compromised site for a future implant.
Injury or Trauma: A hard knock to the mouth can fracture the jaw or damage the tooth socket, causing significant and immediate bone loss that requires intervention.
Any of these scenarios can leave the future implant site too weak for surgery.
Actionable Takeaway: Build a Strong Foundation for Decades of Use
A bone graft rebuilds what was lost, adding volume and density back to the jaw to create a solid, stable base. It acts as a scaffold that encourages your body to grow new, living bone.
This step is critical for ensuring the implant can handle immense daily bite forces. With a strong foundation, the implant can properly fuse with your jaw—the biological key to its permanent success.
The purpose of a bone graft is to transform a compromised site into an ideal one. It prepares the jaw to not just accept an implant but to fully merge with it, creating a single, durable structure that functions like a natural tooth root.
Once your jaw is strong and healthy, you can confidently explore the best options for replacing missing teeth with your dentist.
Comparing the Different Types of Bone Grafts
Your surgeon won't use a one-size-fits-all approach to bone grafting. They will select a graft material perfectly suited to your unique biology, a decision that directly impacts your healing and overall dental bone graft success rate. Understanding the "why" behind their choice helps you become an informed partner in your own care.
The infographic below shows how tooth loss and disease can compromise the jawbone, highlighting why a graft is often essential for giving a dental implant a stable, long-lasting home.
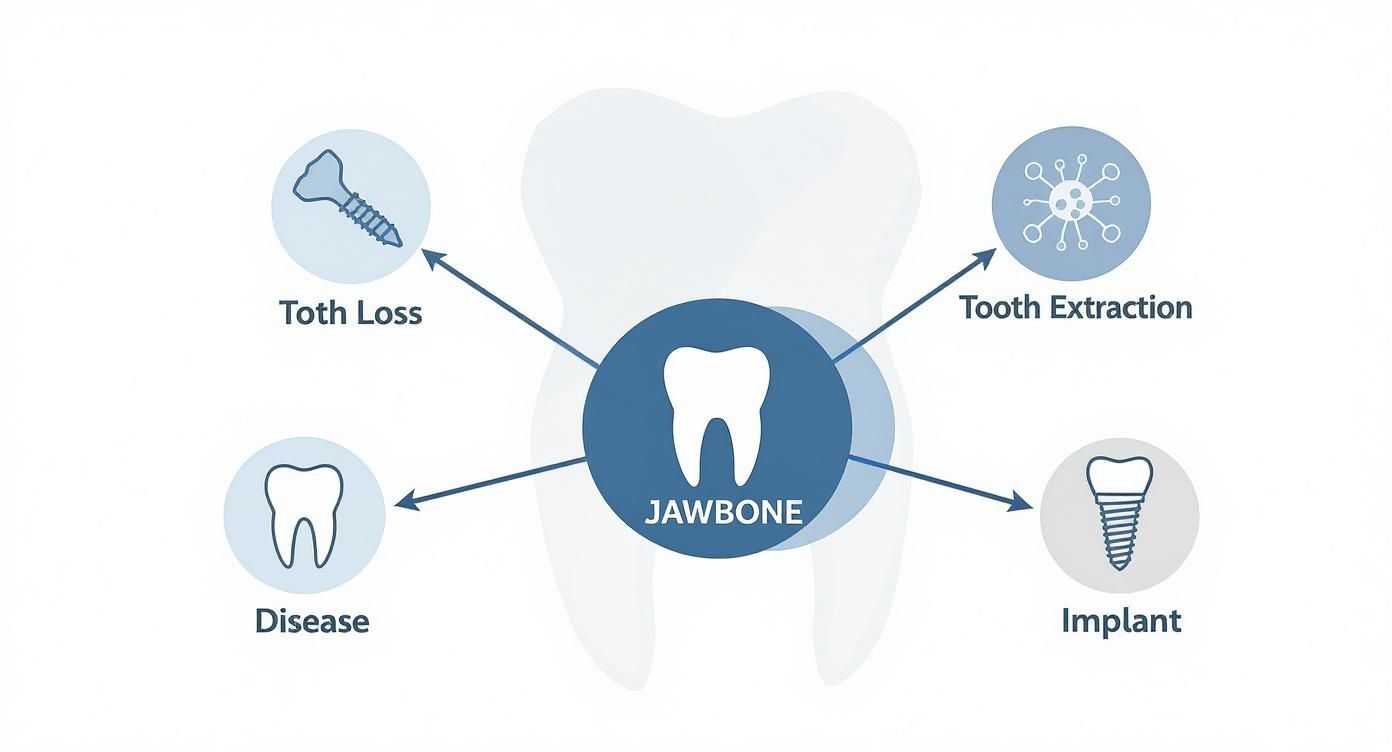
Whether the bone loss is from an extraction or an old infection, the goal is always the same: rebuild the jaw’s foundation so it's strong and sound.
Autografts: The Gold Standard
With an autograft, the bone comes from you, harvested from another spot like your chin or the back of the jaw. It's the gold standard because it contains your own living cells, meaning there’s virtually zero risk of rejection. Your body immediately recognizes it and starts the healing process. The main drawback is the need for a second surgical site, which can add to recovery time.
Allografts: The Reliable Alternative
An allograft uses bone from a human donor, processed and sterilized by a certified tissue bank. All cellular material is removed to eliminate any immune response, making it completely safe. This approach avoids a second surgical site, simplifying the procedure and recovery.
Allografts act as a perfect "scaffold." While they don't contain living cells like an autograft, they provide an ideal framework that encourages your own bone-forming cells to move in, populate the area, and replace it with your own healthy, new bone.
This is an extremely common and highly successful option, often used for routine procedures like socket preservation after an extraction.
Xenografts and Alloplasts: Engineered Solutions
Sometimes, the ideal material isn't human bone at all.
Xenografts are made from an animal source, usually bovine (cow) bone, which is purified to leave just the mineral framework. This structure acts as a fantastic, slow-resorbing scaffold, giving your body ample time to build new bone around it.
Alloplasts are entirely synthetic materials, like calcium phosphates, designed to mimic natural bone. They carry zero risk of disease transmission and are an excellent choice for patients who prefer to avoid biological material.
Your surgeon will recommend the best option based on your clinical needs, ensuring your future implant gets the solid foundation it needs to last a lifetime.
How You Can Directly Influence Your Bone Graft Success
While your surgeon’s skill is critical, you are a key player in your own healing. The choices you make before and after surgery directly impact your dental bone graft success rate. By taking an active role, you create the perfect healing environment inside your body and give the graft the best possible chance to succeed.

Non-Negotiables Before and After Surgery
Certain lifestyle choices can support or sabotage your healing. The single biggest threat is smoking. Nicotine constricts blood vessels, choking off the flow of oxygen and nutrients to the surgical site. This stalls healing, increases infection risk, and can cause the graft to fail. Quitting, even temporarily around your procedure, makes a world of difference.
Additionally, get any systemic health conditions under control:
Control Your Blood Sugar: If you have diabetes, stable blood sugar is non-negotiable. Uncontrolled glucose impairs your immune system and slows healing.
Manage Bone Density: Conditions like osteoporosis can affect jawbone quality, making it harder for the graft to take.
Support Immune Health: A compromised immune system makes you more vulnerable to post-op infection.
Work with your primary care doctor to manage these conditions before surgery. To understand more, read about the link between diabetes and oral health.
Your Actionable Healing Checklist
Following your post-op instructions is your roadmap to success. Here’s a practical checklist to keep you on track.
1. Prioritize Proper NutritionYour body needs the right building blocks to create new bone. Focus on a diet rich in:
Calcium: Dairy, leafy greens, and fortified foods.
Vitamin D: Fatty fish and sunlight to help absorb calcium.
Vitamin C: Essential for producing collagen, the framework for new bone.Stick to soft foods like smoothies, yogurts, and soups initially to avoid pressure on the surgical site.
2. Master Gentle Oral HygieneKeeping the area clean is vital to prevent infection. Do not brush the graft site directly for the first few days. Instead, use the prescribed antibacterial mouthwash to gently rinse the area and protect the healing tissues.
3. Follow Activity RestrictionsStrenuous exercise can spike your blood pressure, causing bleeding or swelling at the graft site. Take it easy for the first week and follow your surgeon’s advice on when to resume normal activities.
Following your surgeon's post-operative instructions is not optional. Each guideline—from medication schedules to diet restrictions—is designed to protect the fragile graft site, prevent complications, and give your body the uninterrupted time it needs to heal properly.
By embracing these steps, you become an active partner in your recovery, directly and positively influencing your dental bone graft success rate and paving the way for a stable, long-lasting dental implant.
What Clinical Studies Reveal About Graft Success
The 95%+ success rate isn't just a guess; it's a figure backed by a mountain of clinical evidence. Digging into the research provides a clearer picture of how bone grafts perform in the real world over many years.
This data helps us understand not just that grafts work, but why they work so well. The overwhelming message from decades of research is one of confidence and reliability.
Long-Term Studies Confirm High Success
Long-term data is the gold standard. A recent 15-year retrospective study of over 450 complex bone grafting procedures found a staggering 98.3% success rate for the grafts themselves. Even better, the dental implants placed into that new bone succeeded 97.2% of the time. This shows that grafts create a truly durable foundation. You can dive into the full details in this study on long-term graft outcomes.
The study also found no significant difference in success between various graft materials, reinforcing a key point: your surgeon's skill in choosing and placing the right material for your situation is what truly drives a successful outcome.
The true value of clinical research isn't just in the final success statistic. It’s in understanding the variables that lead to that success, empowering skilled clinicians to replicate positive outcomes by controlling for factors that could otherwise lead to complications.
The actionable takeaway for you is that the experience of your surgeon matters—a lot. An expert knows how to navigate potential issues identified in clinical research to ensure your success.
Reading Between the Lines: What Research Teaches Us
Good research also highlights situations where success rates might dip. Studies consistently flag the same risk factors—smoking, uncontrolled diabetes, and poor oral hygiene—as the primary culprits behind complications. This is a hard conclusion drawn from observing thousands of patient outcomes.
This research also drives constant improvements in surgical techniques, such as:
Using different membrane types to protect healing grafts.
Determining optimal healing timelines before placing an implant.
Refining surgical approaches to preserve blood supply.
This cycle of research and refinement keeps pushing the dental bone graft success rate even higher.
The Surgeon's Role in Applying Clinical Evidence
An experienced oral surgeon or implant specialist brings the collective knowledge of years of clinical research into the operating room. They know which graft material is best for a specific type of bone loss and how to manage patients with underlying health risks to achieve a predictable, successful outcome. When you choose your surgeon, you're choosing a professional who understands the science behind bone regeneration and can apply it to your personal success story.
Recognizing the Warning Signs of Graft Failure
Knowing the difference between normal healing and a true red flag is crucial for a successful outcome. It puts you in control of your recovery, helping you spot potential issues early.

It is completely normal to experience some soreness, swelling, and minor bruising for a few days after the procedure. These are signs that the healing process has begun. However, some symptoms are not part of the standard healing playbook. If you experience something that feels off, your first action should be to call your surgeon.
Actionable Tip: Differentiate Normal Healing from Red Flags
Normal healing involves gradual improvement each day. Warning signs are symptoms that worsen, become more intense, or appear after you thought you were healing well.
Here’s a clear breakdown of what to watch for:
Pain: Soreness that fades over a few days is typical. Red Flag: Severe, throbbing pain that increases after the third day.
Swelling: Puffiness for the first 48-72 hours is expected. Red Flag: Swelling that worsens after day three or feels hard and hot.
Drainage: Minor oozing in the first 24 hours is fine. Red Flag: Pus (a thick, yellow, or whitish discharge) is a clear sign of infection.
Exposed Graft Material: Feeling a few tiny, sand-like particles is not uncommon. Red Flag: A noticeable chunk of the graft becomes visible through the gums.
A Controversial View on Long-Term Failure
While most studies point to a very high dental bone graft success rate, some dissenting voices exist. Dr. Motiwala, a proponent of "No-Graft Implantology," controversially claims that up to 63% of bone grafts fail or suffer significant loss within five years. This number is far from the >95% success rates seen in most clinical literature and highlights an ongoing debate within the profession. You can read more about this critical perspective on bone graft failure rates to understand the other side of the story.
The most important takeaway is this: Keep a close eye on your healing, but don't try to diagnose yourself. If anything feels wrong or is getting worse instead of better, your only move is to call your surgeon. Catching a problem early is the absolute key to fixing it.
By understanding these warning signs, you can ensure your healing stays on course, setting you up for a strong, stable foundation for your future implant.
Your Top Questions About Dental Bone Grafts, Answered
Knowing the practical, day-to-day details can make you feel more prepared and confident. Here are answers to the most common questions we hear from patients.
How Long Does It Take to Heal?
Healing time varies. For a minor graft, like preserving a socket after an extraction, you might be ready for an implant in 3-4 months. For a more complex procedure like a sinus lift, your surgeon will likely want to wait 6-9 months. This ensures the new bone becomes dense and strong enough to support an implant for life. We will track your progress with X-rays to know exactly when the time is right.
Your body ultimately sets the pace. While we can give you a general timeframe, the final green light for placing an implant comes only when we see solid proof that your new bone is fully mature and up to the task.
What’s the Real Story on Pain and Discomfort?
You won't feel pain during the procedure thanks to modern local anesthesia. Afterward, expect mild soreness and a dull ache for a few days, which is easily managed with over-the-counter medications like ibuprofen. Your surgeon might also provide a prescription for something stronger for the first 48 hours. Actionable Tip: If you experience severe, throbbing pain that worsens after day three, call your surgeon's office immediately, as this is not normal.
What Can I Actually Eat After a Bone Graft?
Your diet is a huge part of protecting the healing graft. For the first two days, stick to cool, soft, and liquid-only foods.
Go-to foods: Smoothies, yogurt, applesauce, and lukewarm soups.
Adding more options: After a couple of days, slowly introduce scrambled eggs, mashed potatoes, and oatmeal.
"Do not eat" list: Avoid chewing directly on the graft site. Stay away from anything hard, crunchy, or sharp (like chips, nuts, or seeds) that could irritate the area and disrupt healing.
Sticking to these simple rules will help make your recovery as smooth as possible.
At Beautiful Dentistry, we know that an informed patient is an empowered one. If you have more questions or you’re ready to discuss a treatment plan tailored to you, our team is here to provide the honest, expert guidance you deserve. Schedule your $59 new patient exam and X-rays today!





Comments