What's a dry socket? An Actionable Guide to Symptoms, Causes, and Prevention
- Caterina Rutter
- 3 days ago
- 12 min read
A dry socket is one of the most painful complications after a tooth extraction. It happens when the protective blood clot in the empty socket gets dislodged or dissolves too soon, leaving the underlying bone and nerve endings exposed. This exposure to air, food, and fluids is what causes the signature, intense pain of a dry socket.
How Your Body Heals After an Extraction
When a tooth is removed, your body immediately starts its natural healing process. The first and most critical step is forming a blood clot in the empty socket. This clot is not just a scab; it’s a vital protective barrier for the sensitive bone and raw nerves underneath.
Think of the blood clot as a natural bandage. It shields the wound and, crucially, provides the foundation for new bone and gum tissue to grow. If this "bandage" is removed prematurely, the entire healing process is disrupted, leading to significant pain and a delay in recovery.
What Goes Wrong with a Dry Socket
When the protective clot is lost, you get alveolar osteitis, more commonly known as a dry socket. Without this natural shield, the exposed bone and nerves become extremely sensitive. Even breathing cool air can trigger a deep, throbbing ache that often radiates toward your ear and down your neck. This is a severe pain, far beyond the normal soreness expected after an extraction.
Dry socket is the most common complication following tooth removal, particularly after wisdom teeth surgery. While it occurs in only about 0.5% of simple extractions, that rate can jump to as high as 30% for surgically removed, impacted wisdom teeth, according to research on dry socket incidence rates.
Actionable Insight: The severe pain of a dry socket is your body's alarm system. It's not just slow healing; it's a direct signal that the critical blood clot is missing. Recognizing this allows you to stop "toughing it out" and seek the dental care you need for relief.
The first few days post-extraction are the most critical. This is the window where you have the most control over preventing this painful complication.
To help you stay on top of your recovery, here’s what to watch for day-by-day.
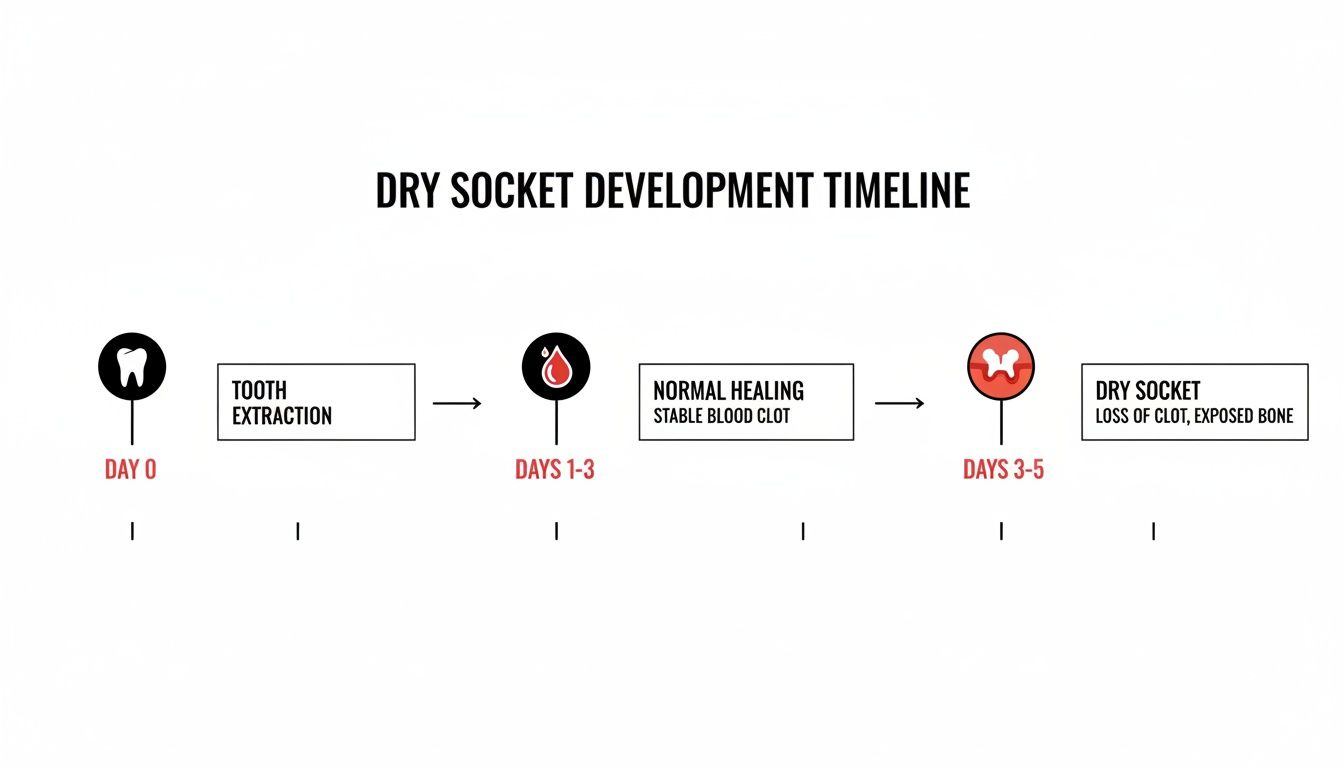
Normal Healing vs Dry Socket Timeline
Timeline After Extraction | Normal Healing Signs (What to Expect) | Dry Socket Warning Signs (When to Call Your Dentist) |
|---|---|---|
First 24 Hours | A dark red blood clot is visible in the socket. Mild to moderate pain and swelling are easily managed with prescribed medication. | The socket appears empty, or the blood clot is not visible. |
Days 1-3 | Pain and swelling should be gradually decreasing each day. The blood clot should remain securely in place. | Pain gets worse instead of better. A bad taste or foul odor starts to develop. |
Days 3-5 | Discomfort continues to fade. The socket begins to look less like a hole and more like it's starting to close. | You experience severe, throbbing pain that may radiate to your ear. The socket looks empty, and you might see visible bone. |
Days 7-10 | You should have minimal to no pain. The socket is visibly healing with new, pink tissue forming. | The pain is still severe and requires professional care. Healing has clearly stalled. |
The key takeaway is the pain trend. In a normal recovery, your discomfort should steadily improve. If your pain suddenly worsens a few days after the procedure, that is a major red flag. Your action step is to call your dentist immediately.
Recognizing the Symptoms of a Dry Socket

It’s normal to have some soreness after a tooth extraction, but the pain from a dry socket is uniquely severe and often delayed. Knowing these specific signs empowers you to identify the problem early and get professional help quickly.
The number one symptom is a severe, throbbing pain that begins a few days after your extraction. This isn't the dull ache of normal healing; it's an intense, persistent pain that over-the-counter medication typically cannot resolve. The pain starts at the extraction site but rarely stays there.
A classic sign of dry socket is radiating pain. The ache often travels from the empty socket up toward your ear, eye, or temple on the same side of your face. If you're experiencing this, it's a strong indicator that you need to contact your dentist.
The Critical Timeline
Timing is a key diagnostic tool you can use yourself. The normal soreness after an extraction peaks within the first 24-48 hours and then steadily improves. A dry socket flips this timeline.
Actionable Insight: The tell-tale pain of a dry socket typically begins two to four days after your tooth was removed. This delay is a critical clue. If your pain was getting better and then suddenly worsens, it’s a powerful signal that the protective blood clot has been lost.
This delayed onset often catches people by surprise. If your recovery takes a sudden turn for the worse, don't dismiss it. It's your cue to take action.
Visual and Sensory Clues
While pain is the primary symptom, there are other signs you can check for. Gently pull back your cheek and look at the extraction site in a well-lit mirror. The socket might look disturbingly empty. Instead of a dark blood clot, you might see a hollow-looking hole.
In some cases, you may even see the whitish glint of the jawbone. Seeing exposed bone is a definitive sign of a dry socket. This is often accompanied by other unpleasant symptoms.
Here is a checklist of additional signs to watch for:
Foul Taste: A persistent, nasty taste in your mouth that rinsing doesn't fix.
Unpleasant Odor: Bad breath that seems to come directly from the extraction site, often caused by trapped food and bacteria.
Swollen Glands: You may notice tenderness or slight swelling in the lymph nodes in your neck or under your jaw.
When you combine the signature severe, radiating pain with these visual and sensory clues, the diagnosis becomes clear. Recognizing these symptoms gives you the confidence to stop wondering and call your dentist for immediate relief.
Key Risk Factors for Developing a Dry Socket
While anyone can develop a dry socket, certain factors significantly increase your risk. Knowing these risks is your first line of defense, empowering you to take proactive steps for a smoother, less painful recovery.
Some of the most significant risks are related to your daily habits—things you have direct control over. These actions can physically dislodge the protective blood clot or introduce chemicals that interfere with your body's healing process.
Your Habits and Actions Matter
The most common culprits create suction in your mouth, which can act like a tiny vacuum, pulling the delicate blood clot from the socket. Additionally, certain chemicals can either dissolve the clot or prevent it from forming correctly.
Here are the key habits to manage for a successful recovery:
Smoking and Tobacco Use: The act of inhaling creates powerful suction. Beyond that, nicotine constricts blood vessels, reducing blood flow and slowing healing. This double-threat makes smoking the single biggest controllable risk factor. Your Action: Stop smoking for at least 48 hours before and 72 hours after your extraction.
Using a Straw: Sipping through a straw creates the same vacuum effect that can easily dislodge the clot. Your Action: Drink directly from a glass.
Spitting or Rinsing Too Hard: Forceful spitting or swishing can create enough pressure to disturb the healing site, especially within the first crucial 72 hours. Your Action: When you rinse, let the water gently fall out of your mouth into the sink.
Actionable Insight: Understand that simple physical forces can sabotage your recovery. Avoiding any form of suction is a non-negotiable rule for the first few days. Making a conscious choice to pause these habits is the most impactful thing you can do to prevent a dry socket.
Biological and Procedural Factors
Other risks are tied to your personal biology or the nature of your dental procedure. It is crucial to discuss these with your dentist beforehand so you can receive aftercare instructions tailored to your specific needs.
These factors include:
Difficult Extractions: A complex procedure, such as removing an impacted wisdom tooth, involves more trauma to the bone and gum tissue, naturally increasing the risk of a dry socket. Our guide on what to expect during wisdom teeth removal explains this in more detail.
Past History: If you've had a dry socket before, you are more likely to experience it again. Inform your dentist of this history.
Oral Contraceptives: High estrogen levels from some birth control pills can interfere with blood clot formation. Your Action: Discuss timing your extraction with your dentist and primary care physician.
Poor Oral Hygiene: Pre-existing infections or high levels of bacteria in the mouth can contaminate the extraction site and prevent a stable clot from forming.
Being aware of these risks allows you to have a proactive conversation with your dentist and take targeted steps to prevent this painful complication.
How Dentists Treat a Dry Socket
If you suspect you have a dry socket, your first and most important action is to call your dentist. Self-treatment is not effective for this level of pain; professional care can provide almost immediate relief. The treatment goal is simple: clean and protect the exposed area so your body can resume healing.
In-Office Care: Getting You Comfortable Again
The first thing your dentist will do is gently clean the socket. This step is essential, as food particles and bacteria can become trapped in the empty space, causing irritation and preventing healing. The area will be carefully flushed out to ensure it is completely clean.
Next, your dentist will place a special medicated dressing directly into the socket to soothe the exposed nerves and protect the bone.
Actionable Insight: This medicated dressing is the key to your relief. It's often made with ingredients like eugenol (from clove oil), which has natural analgesic and antiseptic properties. It acts as a temporary replacement for the lost blood clot, immediately shielding the sensitive nerve endings from air and other irritants.
Most patients feel a significant reduction in pain almost as soon as the dressing is in place. You may need to return for a dressing change every day or two until the pain subsides and healing is well underway.
Supporting Your Recovery at Home
While in-office care is critical, your actions at home are equally vital for a successful recovery. Your dentist will provide specific instructions, but they will center on pain management and keeping the area clean.
Here are the practical steps you'll need to follow at home:
Continue Gentle Salt Water Rinses: Gently rinsing with warm salt water, especially after meals, helps keep the socket clean without disturbing the new dressing. Remember to let the water fall out of your mouth—no forceful spitting.
Use Cold Packs: Apply a cold pack to the outside of your jaw for 15-20 minutes at a time. This can help reduce any residual swelling and numb the throbbing pain.
Follow Pain Management Instructions: Take pain relief medication exactly as directed by your dentist. This may be an over-the-counter anti-inflammatory or a stronger prescription pain reliever for the first few days.
Healing from a dry socket requires teamwork between you and your dentist. For those interested in the science of wound management, exploring advanced wound care treatment options can provide further insight. By diligently following your dentist's plan, you will effectively manage the discomfort and get your recovery back on track.
Actionable Steps You Can Take to Prevent a Dry Socket
While a dry socket can be intensely painful, the good news is that it is almost always preventable. By taking a few simple, proactive steps before and after your tooth extraction, you can protect the vital blood clot and ensure a smooth, comfortable healing process.
Treat the first 72 hours after your procedure as the "clot protection zone." During this critical window, the clot is extremely fragile. Your primary mission is to avoid anything that creates suction or pressure in your mouth, as these forces are the main reasons healing fails.
Before Your Tooth Extraction
Your prevention strategy begins before you even sit in the dental chair. A proactive conversation with your dentist is your most powerful tool. They can help create a personalized prevention plan based on your health history and risk factors. Effective patient engagement through effective patient education resources is proven to improve outcomes.
Take these key actions beforehand:
Discuss Your Medications: Provide your dentist with a complete list of all medications you take. Oral contraceptives, for example, can affect clotting, and your dentist needs to know this.
Stop Using Tobacco: If you smoke or use tobacco, it is crucial to stop for at least a day before surgery and for as long as possible afterward.
Prepare Your Recovery Kit: Stock your kitchen with soft foods and clear your schedule of strenuous activities for a few days. For more tips, use our actionable checklist for oral surgery preparation.
After Your Tooth Extraction
Once the tooth is removed, your entire focus should shift to gentle, mindful aftercare. Your habits over the next three days will directly impact the success of your recovery.
Actionable Insight: The most common causes of a dislodged blood clot are physical forces. For at least three days, your rulebook is simple: no straws, no smoking, and no forceful spitting.
Adhere to these guidelines to keep your recovery on track:
Eat Soft Foods: Stick to easy-to-eat foods like yogurt, applesauce, mashed potatoes, and lukewarm soups.
Stay Hydrated: Drink plenty of water to support your body’s natural healing processes.
Rinse Gently: After the first 24 hours, you can begin gently rinsing with warm salt water. The key is to tilt your head and let the water fall out of your mouth into the sink—no swishing or spitting.
Avoid Straws Completely: The suction from using a straw is a primary cause of dislodged clots.
Do Not Smoke or Vape: This creates dangerous suction and the chemicals severely delay healing.
Your Dry Socket Prevention Checklist
Use this checklist to guide you. Following these steps dramatically reduces your risk of complications.
Action Item | Why It's Important (The "Actionable Insight") | When to Do It |
|---|---|---|
Discuss medications with your dentist | Informs your dentist of risks (e.g., birth control) so they can advise you. | During your consultation |
Pause tobacco and nicotine use | Directly prevents harmful suction and allows proper blood flow for healing. | At least 24 hours before & 72+ hours after |
Stock up on soft foods | Removes the temptation to chew hard foods that can dislodge the clot. | The day before your extraction |
Avoid straws completely | Eliminates the number one cause of suction-related clot dislodgement. | For at least the first 72 hours |
Do not spit or swish forcefully | Prevents creating pressure that can push the clot out of the socket. | For at least the first 72 hours |
Rinse gently with salt water | Cleans the area safely without disturbing the fragile healing site. | Starting 24 hours after extraction |
Avoid strenuous physical activity | Keeps blood pressure stable to prevent bleeding and dislodging the clot. | For the first 48-72 hours |
Taking these targeted steps is the most effective way to ensure your recovery is quick, uneventful, and free from the avoidable pain of a dry socket.
How We Help You Avoid and Treat Dry Socket
Your best defense against complications like dry socket is having an expert dental team dedicated to your successful recovery. At Beautiful Dentistry, our entire approach is designed to prevent problems before they start, ensuring your healing is as smooth and pain-free as possible.
Prevention begins with the extraction itself. We employ gentle, precise surgical techniques that minimize trauma to the surrounding bone and gum tissue. A less traumatic procedure gives your body the best possible chance to form a stable, protective blood clot.
We believe in personalized care, not "one-size-fits-all" instructions. Before your procedure, we'll review your specific risk factors—from medications to daily habits—and create a tailored recovery plan with you. You will leave our office with clear, actionable instructions, eliminating any guesswork during your recovery.

Our Commitment to Your Recovery
Even with the best prevention, complications can sometimes occur. If you experience the warning signs of a dry socket, we are committed to providing fast, effective care to relieve your pain. We understand how distressing this condition is, and we will ensure you get the immediate attention you need.
Our proactive approach includes:
Thorough Pre-Operative Planning: We identify your individual risks and create a clear prevention strategy you can follow.
Gentle Surgical Methods: Our experienced team focuses on minimally invasive techniques to protect the delicate healing area.
Clear Aftercare Guidance: We provide simple, easy-to-follow instructions that empower you to take control of your recovery.
Our Philosophy: Proactive, patient-focused care is the key to preventing dry socket. By combining skillful surgery with personalized education and unwavering support, we empower you to heal correctly and confidently.
This careful, methodical approach is central to all our services, including our tooth removal and extractions in Tempe.
Your Dry Socket Questions Answered
It’s normal to have questions. Here are clear, actionable answers to the most common concerns we hear from patients.
Can a Dry Socket Heal on Its Own?
While the body will eventually heal the area, leaving a dry socket untreated is a painful and prolonged ordeal. Without intervention, you face an excruciatingly slow healing process.
The Actionable Step: See your dentist immediately. We will clean the socket and place a medicated dressing. This single action protects the exposed bone, provides immense pain relief, and accelerates your healing.
How Long Does Dry Socket Pain Last?
If left untreated, the severe pain of a dry socket can last for 7 to 10 days or even longer.
With proper dental treatment, however, relief is rapid. After the socket is cleaned and dressed, most patients experience a dramatic reduction in pain. The intense, radiating ache should calm down significantly within 24 to 48 hours of your dental visit.
Actionable Insight: The goal of treatment is to stop the severe pain quickly. While the socket itself still needs a couple of weeks to fully heal, the unbearable pain you're feeling should resolve almost immediately after a dentist protects the exposed bone with a medicated dressing.
Can I Get a Dry Socket a Week After an Extraction?
This is extremely unlikely. The critical risk period for developing a dry socket is within the first 2 to 4 days after surgery, when the initial blood clot is most fragile.
By the one-week mark, your body’s healing process is well underway. The clot has started to be replaced by new granulation tissue, making the site much more stable and secure. If you develop new pain after a week, call your dentist, but it is unlikely to be a dry socket.
At Beautiful Dentistry, our care continues until you are fully healed and comfortable. If anything feels wrong after your extraction or you experience unexpected pain, do not wait. Call us immediately. Your health and comfort are our top priorities.
Ready to schedule your appointment? Visit us at https://zdentist.com.


Comments