What Does a Dry socket Feel Like? Pain, Symptoms & Healing
- Caterina Rutter
- Oct 16, 2025
- 11 min read
So, you've had a tooth pulled, and you're expecting to feel better day by day. But what if the pain suddenly takes a sharp turn for the worse? That's often the first sign you're dealing with something more than normal recovery. A dry socket feels like a deep, throbbing ache that seems to come out of nowhere, steadily intensifying instead of fading away.
This isn't just a little soreness. The pain often radiates from the empty socket, traveling up your jaw toward your ear, eye, or temple on that side of your face. It's a uniquely severe discomfort, almost like an exposed nerve getting zapped by cold air. If this sounds familiar, your immediate action should be to contact your dentist.
The Telltale Signs of a Dry Socket
After an extraction, your body’s natural healing process kicks in by forming a blood clot in the empty socket. This clot is a critical, protective bandage covering the underlying bone and sensitive nerve endings.
A dry socket, or alveolar osteitis as it's known medically, happens when that critical blood clot gets dislodged, dissolves, or never forms properly. This complication typically arises 2 to 4 days after the procedure—precisely when you should be feeling better.
Without that protective layer, the bone and nerves are left exposed to air, food, and fluids. This exposure is the direct cause of the intense, throbbing pain that over-the-counter medication barely touches. For more in-depth information, you can discover more research about this condition on journals.sagepub.com.
Distinguishing Normal Healing from a Problem
It’s completely normal to have some soreness after a tooth extraction. The key is that this discomfort should gradually decrease each day. Dry socket pain is different; it shows up unexpectedly and ramps up quickly, feeling far worse than the initial pain from the surgery itself.
Actionable Insight: The key difference is the timing and intensity. If your pain suddenly escalates a few days after your extraction instead of fading away, it's a major red flag. Your next step should be to call your dentist immediately.
To help you tell the difference, here's a quick comparison of what to expect.
Dry Socket Pain vs Normal Healing Pain
Symptom | Normal Healing Pain | Dry Socket Pain |
|---|---|---|
Pain Level | Mild to moderate, manageable with prescribed medication. | Severe, throbbing, and often unresponsive to painkillers. |
Timeline | Peaks within the first 24-48 hours and then steadily improves. | Begins 2 to 4 days after the extraction and gets progressively worse. |
Location | Centered around the extraction site. | Radiates from the socket to the ear, eye, temple, and neck. |
Appearance | A dark blood clot is visible in the socket. | The socket looks empty, and you may see whitish bone. |
Other Signs | Mild swelling and bruising that slowly fade. | Foul odor from the mouth and an unpleasant taste. |
This table makes it clear that while some pain is part of the package, the intense, delayed, and radiating pain of a dry socket is in a category of its own.
Beyond the pain itself, you can perform a quick self-check for these other clear signs:
Visible Bone: Look in the mirror with a flashlight. Do you see a whitish, bony surface instead of a dark, healthy-looking blood clot?
Foul Odor: Is there a persistent bad smell coming from your mouth, even after gentle rinsing?
Bad Taste: Do you have a nasty, lingering taste that just won't go away?
Catching these signs early is the most important step toward getting treatment and, more importantly, getting relief. If you identify any of these symptoms, your next move is to call your dentist.
Why a Missing Blood Clot Causes Severe Pain
Think of the blood clot that forms after a tooth extraction as a natural, protective bandage. It’s a lot like a scab that forms over a scraped knee. Its whole job is to shield the underlying bone and the incredibly sensitive nerve endings from everything going on inside your mouth.
When that crucial clot gets knocked loose or dissolves before it's supposed to, it leaves those raw tissues completely exposed. Suddenly, air, food particles, and bacteria can get right down into the socket, which is what causes the signature, throbbing pain of a dry socket.
This simple timeline below shows how the whole process unfolds, from a healthy start to a painful problem.
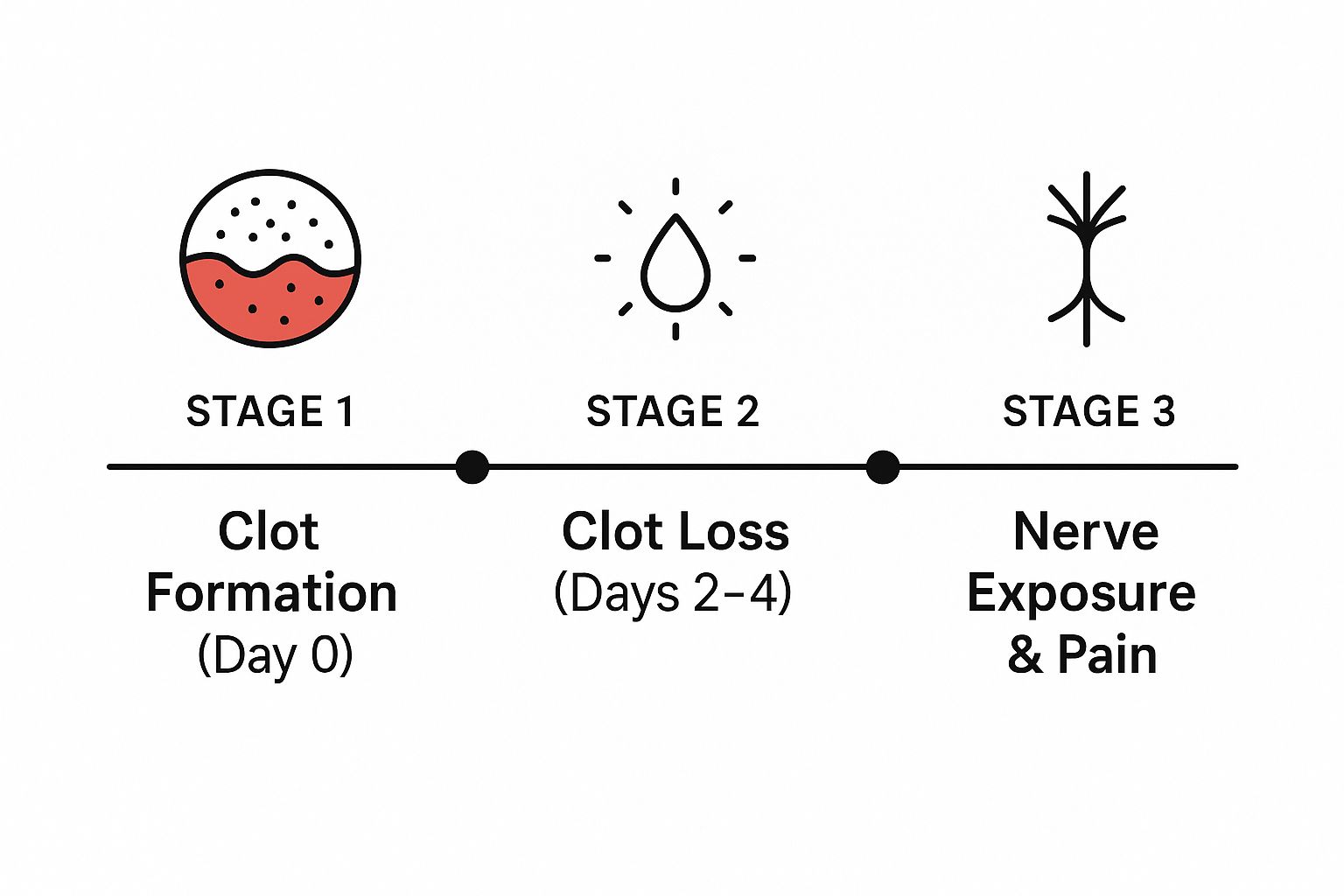
As you can see, the issue isn't something that happens right away. The real trouble starts a few days after the procedure, once that protective clot is gone and the nerve exposure begins.
The Role of the Exposed Nerve and Bone
Once the nerves in your jawbone are out in the open, they become hyper-sensitive. Something as simple as breathing in cool air or taking a sip of water can send waves of intense pain through your jaw. The bone itself was never meant to be exposed, so it becomes inflamed, adding to that deep, aching feeling that seems to radiate outward.
Actionable Insight: The pain is not an infection but a raw nerve reaction. This is why standard painkillers often fail to provide relief. Don't waste time trying different over-the-counter options; professional treatment that covers the nerve is the only effective solution.
Understanding this biological breakdown makes it clear why dry socket pain is so different. It’s not just a normal part of healing; it’s a blaring signal that the healing process has been seriously derailed. Getting professional care is the only way to cover that exposed area, calm down the irritated nerves, and finally get your healing back on track.
The Timeline: When Dry Socket Pain Hits
One of the sneakiest things about a dry socket is its timing. After a tooth extraction, you expect some discomfort. Typically, that pain is at its worst for the first 24 to 48 hours and then slowly starts to get better each day. That’s the normal healing process.
A dry socket, however, completely flips that script. Just when you think you’re turning a corner, the pain roars back, often worse than it was right after the surgery. This sudden reversal is your biggest clue that something isn't right.
The Tell-Tale Delay in Pain
The pain from a dry socket doesn't show up on day one. It almost always makes its grand entrance between the second and fourth day following your extraction. This delayed onset is what really sets it apart from the usual post-op soreness.
So, if you’re on day three and the pain is getting dramatically worse instead of better, that’s a massive red flag. It’s a strong signal that the protective clot is gone and the socket is exposed.
How the Pain Gets Worse
Without that blood clot acting as a natural bandage, the underlying bone and nerve endings are left open to everything in your mouth—air, food, liquids. This exposure leads to intense irritation.
The pain doesn't just get stronger; it changes. It often becomes a deep, throbbing ache that can radiate from the socket up to your ear, eye, or temple on that side of your face. This isn't just a little soreness; it's a clear sign that the healing site has been disturbed and needs immediate attention.
Actionable Insight: Monitor your pain daily. If your pain level is higher on day 3 or 4 than it was on day 2, stop waiting for it to improve. This is your cue to call your dentist’s office for an evaluation.
Studies tracking patient experiences confirm this timeline. For example, one clinical review found that while 20.6% of patients reported dry socket symptoms within the first two days, that figure jumped to 41.2% by the two-week mark if left untreated. This shows that the pain doesn't just stick around; it intensifies over time. You can read more about these clinical findings on pmc.ncbi.nlm.nih.gov.
Understanding this timeline is crucial, as it helps you know when to stop waiting it out and start seeking help.
Key Risk Factors for Developing a Dry Socket

It’s one thing to know what a dry socket feels like, but it’s far more helpful to know if you might be susceptible in the first place. You can actively reduce your risk by managing specific behaviors and discussing your health history with your dentist before your procedure.
The most common cause is creating suction in your mouth. Actions like sipping from a straw or smoking generate negative pressure, which can physically pull the delicate blood clot out of the socket.
Surgical Complexity and Location
Not all tooth extractions are created equal. The difficulty of the procedure and where the tooth was located play a huge role in your risk for developing a dry socket.
For instance, removing an impacted wisdom tooth is a much more involved surgical procedure than a simple extraction. It often involves more trauma to the surrounding jawbone and gums, which naturally makes healing a bit more complicated and raises the risk.
The numbers back this up. One study found that surgical extractions had a prevalence of 6.88% for dry socket, while simple extractions were far lower at just 0.77%. The location is also key; the lower jaw has less blood supply than the upper jaw, making it a more common spot for this problem to occur.
Actionable Insight: Before your extraction, ask your dentist about your specific risk level based on the procedure's complexity. If you are high-risk (e.g., wisdom tooth removal), be extra diligent with your post-op care.
Habits and Health Conditions
What you do after the procedure can either help or hinder your healing. Smoking is a major risk factor for several reasons. It reduces blood flow to the healing area and the chemicals in cigarettes can contaminate the site. For a deeper look, you can read about the overall health risks of smoking.
Beyond smoking, you can take control of these other factors:
Poor oral hygiene: Maintain gentle care around the site to prevent bacteria from disrupting the healing process.
Vigorous rinsing or spitting: Avoid these actions for at least 72 hours to protect the clot.
These are often part of a broader pattern of bad habits that could harm your teeth and your overall oral health.
Knowing about these risk factors ahead of time empowers you. You can talk with your dentist to map out a recovery plan that minimizes these risks and sets you up for a fast, comfortable healing experience.
Actionable Steps to Prevent a Dry Socket

Alright, now that we’ve covered what a dry socket is and why it happens, let's get practical. How do you actually stop it from happening in the first place?
The good news is, you have a lot of control here. A few simple precautions during that first week post-extraction make all the difference in protecting the fragile blood clot your body is working so hard to form.
Your primary goal is to be incredibly gentle and, most importantly, avoid any suction or pressure in your mouth for at least the first 72 hours.
Your Post-Extraction Care Checklist
Following these tips is the single best thing you can do to lower your risk. It’s all about helping that protective blood clot stay put so your body can heal without a hitch.
No Straws, No Smoking: This is non-negotiable. The sucking motion from using a straw or smoking creates powerful negative pressure in your mouth. This is the #1 preventable cause of a dislodged blood clot.
Embrace Soft Foods: For the first few days, stick to a soft-food diet. Choose yogurt, applesauce, mashed potatoes, or smoothies. Actively avoid anything hard, crunchy, or chewy that might get lodged in the socket.
Gentle Oral Hygiene is Key: You can and should brush your other teeth, but give the extraction site a wide berth. To rinse, do not swish or spit. Instead, gently tilt your head and let a warm saltwater solution flow out of your mouth over the sink. This keeps the area clean without applying force.
Actionable Insight: The game plan is to keep the environment in your mouth calm and stable. Before you do anything—eat, drink, or clean—ask yourself: "Does this create suction, pressure, or could it poke the healing socket?" If the answer is yes, don't do it.
Why You Need to Take It Easy
Don't underestimate the power of rest. It’s critical to avoid any strenuous activity for the first few days after your procedure.
Hitting the gym or doing any heavy lifting can spike your blood pressure. That increased pressure can make the extraction site throb and potentially dislodge the clot. Give your body a break—it's using that energy to heal.
How to Find Relief from Dry Socket Pain
If you think you have a dry socket, the single most important thing you can do is call your dentist right away. This isn't something you can just "tough out." Professional treatment is the only real path to getting relief and making sure the area heals correctly.
When you get to the office, the first thing your dentist will do is gently clean out the socket. This crucial step removes any food debris or contaminants that are causing irritation and pain.
What to Expect During Treatment
Once the socket is clean, your dentist will apply a medicated dressing. This isn't just a regular piece of gauze; it's a special paste or a small strip soaked in ingredients like eugenol (which comes from clove oil) to soothe the area.
You'll be amazed at how quickly this works. For most people, the relief is almost immediate. The dressing acts like a protective seal, covering up that exposed bone and those raw nerve endings. It’s the fastest way to stop that deep, throbbing ache.
Actionable Insight: The primary goal of professional treatment is to protect the exposed socket, manage pain, and allow your body’s natural healing process to get back on track. Do not attempt home remedies; seek professional care for the quickest and safest relief.
Managing Pain Until Your Appointment
That waiting period before you can see your dentist can feel like an eternity when you're in so much pain. Here are a few things you can do at home to take the edge off in the meantime:
Over-the-Counter Pain Relievers: Take an anti-inflammatory like ibuprofen to help reduce both pain and swelling, following the package directions.
Cold Compress: Hold a cold pack or ice wrapped in a towel against the outside of your jaw for 15-20 minutes at a time to help numb the area.
Gentle Rinsing: You can carefully rinse your mouth with warm salt water. The key word here is gently—let the water fall out of your mouth rather than spitting.
For urgent advice when you're dealing with severe pain, a doctor on call service can sometimes provide guidance while you're waiting for your dental appointment. The aftercare is pretty simple, too, and has a lot in common with the instructions in our guide to the stages of root canal therapy and aftercare.
Your Top Questions About Dry Socket Answered
We've walked through the what, when, and why of dry sockets, but I know you probably still have some lingering questions. Let's tackle some of the most common concerns I hear from patients so you can feel confident and prepared for your recovery.
How Long Does Dry Socket Pain Actually Last?
If left untreated, the intense, radiating pain of a dry socket can last for 7 to 10 days, or even longer, as the exposed bone slowly gets covered by new tissue.
However, with professional treatment, relief is almost immediate. As soon as your dentist cleans the socket and places a medicated dressing, the severe throbbing pain usually fades within a few hours. This is the most effective action you can take to stop the pain.
Will a Dry Socket Just Heal on Its Own?
Technically, yes, the body will eventually heal the area. But "eventually" is the key word, and it’s a path filled with unnecessary agony. Trying to tough it out is a bad idea—it just prolongs the pain and increases the risk of infection.
Actionable Insight: Do not wait for it to heal on its own. Getting prompt dental care is the only reliable way to stop the pain, prevent complications, and ensure the socket heals correctly.
Is It Okay to Use Clove Oil for the Pain?
I see this question a lot online. While it's true that some professional dental dressings contain eugenol (which comes from clove oil) for its numbing effect, you should never put pure clove oil in the socket yourself.
It’s far too potent and can cause a nasty chemical burn on the fragile tissues, making everything much worse. Please, leave the medicating to your dentist.
For more tips on keeping your mouth healthy, take a look at these frequently asked questions about oral care habits.
Can I Get a Dry Socket After a Filling or Root Canal?
Nope, not a chance. A dry socket is exclusively a complication of tooth extraction.
The whole problem starts when the protective blood clot is lost from an empty tooth socket. Procedures like fillings and root canals don't leave an open socket behind, so there is zero risk of getting a dry socket from them.
If you're dealing with severe pain or are worried about how you're healing after an extraction, don't wait and wonder. The team at Beautiful Dentistry is ready to provide the expert care you need for immediate relief. Contact us today to schedule your appointment and get back to healing comfortably. You can learn more by visiting us at https://zdentist.com.

