What Causes Sleep Apnea in Adults: A Guide to the Real Reasons
- Caterina Rutter
- 4 days ago
- 12 min read
Sleep apnea is more than just loud snoring; it’s a serious condition where your breathing repeatedly stops and starts all night long. These dangerous pauses are caused by one of two core issues: a physical blockage in your airway or a missed signal from your brain telling you to breathe. Understanding which one is affecting you is the first step toward getting the restorative sleep you need.
What’s Really Happening When You Stop Breathing at Night?
When you fall asleep, your muscles relax, including those that hold your throat open. For someone with sleep apnea, this natural process triggers a disruptive cycle. Each breathing pause, known as an apneic event, causes the oxygen level in your blood to drop. Your brain senses this danger and sends an emergency signal to jolt you awake just enough to gasp for air.
This life-saving reflex is so quick you likely won't remember it, but it can happen hundreds of times a night, preventing you from ever reaching deep, restorative sleep. It’s why you can spend a full eight hours in bed yet wake up feeling exhausted. Your body is too busy fighting for air to truly rest and repair itself.
The Three Main Types of Sleep Apnea
To find the right solution, you first need to understand the root cause. Each type of sleep apnea has a different origin, requiring a different approach.
Obstructive Sleep Apnea (OSA): This is the most common form. It’s a physical problem where the soft tissues at the back of your throat, like your tongue or soft palate, collapse during sleep and block your airway.
Central Sleep Apnea (CSA): This is a communication problem. The airway is open, but the brain fails to send the proper signals to the muscles that control breathing.
Complex or Mixed Sleep Apnea: This is a hybrid condition where a person experiences both physical blockages (OSA) and missed brain signals (CSA).
Why Do These Pauses Matter So Much?
These nightly breathing interruptions have serious consequences beyond just feeling tired. Each time you stop breathing, you put immense stress on your cardiovascular system. Over time, this repeated oxygen deprivation becomes a major risk factor for high blood pressure, heart disease, stroke, and type 2 diabetes.
The constant cycle of stopping and starting to breathe is like forcing your body to run a marathon every single night. This nightly stress has a cumulative effect, contributing to long-term health issues and dramatically reducing your quality of life.
The most critical action you can take is to learn the warning signs. If you're concerned, exploring the main symptoms of sleep apnea will give you a clearer picture. Knowing the cause and the symptoms empowers you to have a productive conversation with your doctor and find the right solution.
What's Physically Happening During Obstructive Sleep Apnea?

To get to the bottom of what causes obstructive sleep apnea, we need to look at what physically creates that roadblock in your throat. When you sleep, the muscles holding your airway open relax. For people with OSA, this relaxation causes the airway to narrow or collapse completely, cutting off airflow. Let's break down the factors that contribute to this "plumbing issue" in your upper airway.
Excess Body Weight and Airway Compression
Excess body weight is the most significant and controllable risk factor for OSA. Fatty tissue doesn't just accumulate around your waist; it also builds up in the soft tissues of the neck and tongue. This extra weight puts direct pressure on your airway, narrowing the passage and making it more likely to collapse during sleep.
Obesity is the top modifiable risk factor. A 2019 global study estimated that 936 million adults suffer from mild to severe OSA, with body mass index (BMI) being a primary driver. For men with a BMI over 40, the likelihood of having moderate to severe OSA can be over 50%. This highlights a clear action item: for many, weight management is a powerful first step in treating sleep apnea.
Your Natural Anatomy and Its Role
Even at a healthy weight, your natural anatomy can predispose you to OSA. Certain physical traits can create a natural bottleneck in your airway. Understanding if you have these traits can help you and your doctor pinpoint the cause of your symptoms.
Common anatomical risk factors include:
A Recessed Jaw (Retrognathia): A lower jaw that is set back reduces the space behind your tongue, pushing it closer to your airway.
Large Tonsils and Adenoids: These can act like pillows on either side of your throat, narrowing the passage for air.
A Large Tongue (Macroglossia): A tongue that is proportionally too large for your mouth can easily fall back and block your airway during sleep.
A Narrow Palate: A high, arched roof of your mouth can reduce the overall size of your airway, making obstruction more likely.
If you have one or more of these traits, your airway has less room for error. Normal muscle relaxation during sleep can be enough to trigger a collapse.
How Lifestyle Choices Affect Your Airway
Beyond weight and anatomy, certain daily habits can cause or worsen OSA by excessively relaxing your throat muscles. Identifying and modifying these habits can provide immediate improvement.
Think of your throat muscles as the scaffolding that holds your airway open. Lifestyle choices like drinking alcohol act like a wrecking ball, weakening that support structure and leaving the airway vulnerable to collapse.
Alcohol, especially before bed, is a potent muscle relaxant. It causes the tissues in your throat to become floppy, leading to loud snoring and potential collapse. Sedatives and certain medications, including some sleep aids, have the same effect and can turn mild snoring into full-blown OSA.
Finally, your sleep position is a critical, actionable factor. Sleeping on your back allows gravity to pull your tongue and soft palate directly into your airway. Learning to sleep on your side can open things up significantly. You can find practical tips by learning about the best sleep position for breathing.
Exploring Your Personal Risk Factors for Sleep Apnea
While a physical blockage is the immediate cause of an apnea event, several personal factors can increase your risk. Understanding these factors isn't about worry; it's about arming yourself with knowledge for a productive conversation with your doctor or dentist. This awareness helps you identify your specific risk profile and take targeted action.
The Unavoidable Factors: Age and Gender
As we age, our muscle tone naturally decreases, including in the throat. This can make the airway muscles too weak to stay open during sleep. While you can't stop aging, knowing this can prompt you to be more vigilant about other modifiable risk factors.
Gender also plays a key role. Men are diagnosed with sleep apnea two to three times more often than women before menopause, partly due to hormonal differences and fat distribution patterns. However, this gap closes after menopause. As women's progesterone and estrogen levels decline, their risk for sleep apnea increases to become similar to men's.
Your Family History and Genetics
Inherited traits like a small jaw, a high-arched palate, or the overall shape of your skull can directly impact airway size. If sleep apnea runs in your family, you may have inherited an anatomical structure that makes you more susceptible.
Genetics deals you a specific hand of cards when it comes to airway anatomy. If you inherit a naturally smaller or more crowded airway, there's simply less wiggle room, making you more vulnerable to blockages even at a healthy weight.
While you can't change your genes, knowing your family history is a powerful piece of information to share with your healthcare provider. It helps them connect the dots faster and recommend appropriate screening.
The Connection to Other Health Conditions
Sleep apnea often coexists with other medical issues. Managing these conditions can be a crucial part of managing your sleep apnea.
Here are a few health problems that are frequently linked to sleep apnea:
Hypothyroidism: An underactive thyroid can cause tissue swelling in the throat and tongue enlargement, physically narrowing the airway.
Polycystic Ovary Syndrome (PCOS): The hormonal imbalances and higher likelihood of being overweight associated with PCOS are major risk factors for OSA in women.
Congestive Heart Failure: This condition can cause fluid buildup around the lungs and airway, a known trigger for central sleep apnea.
Chronic Nasal Congestion: If allergies or a deviated septum force you to breathe through your mouth, it alters your jaw position during sleep, making your airway more prone to collapse.
Even chronic teeth grinding (bruxism) can be a red flag; sometimes, the body subconsciously clenches the jaw to keep the airway from collapsing. For actionable advice on this, check out our guide on how to prevent teeth grinding at night.
How Your Dentist Can Be Your First Line of Defense
It may seem unusual to discuss sleep problems at a dental appointment, but dentists are uniquely positioned to spot the early warning signs of sleep apnea. During a routine exam, we get a clear view of your oral anatomy, which often reveals clues about what’s happening to your airway when you sleep. Recognizing these signs is the first actionable step toward diagnosis and treatment.
What We See: The Oral Clues of a Struggling Airway
When we examine your mouth, we're looking for specific red flags that suggest a potential breathing obstruction. These signs can be your body's early warning system.
Here are tell-tale signs we are trained to identify:
Excessive Teeth Grinding (Bruxism): Worn, flat, or chipped teeth are a major indicator. This grinding is often your body's subconscious reflex to tense the jaw muscles and reopen a collapsing airway.
A Scalloped Tongue: Wavy indentations along the sides of your tongue suggest it's too large for your jaw, making it more likely to block your throat at night.
A High, Narrow Palate: The shape of the roof of your mouth is linked to the size of your nasal passages. A high, vaulted palate often means a more crowded airway.
Throat Redness and Irritation: Chronic redness in the soft palate and uvula is a physical sign of the intense vibration from heavy snoring and the stress of the airway repeatedly collapsing and reopening.
Think of your dentist as an airway detective. We're gathering clues from your teeth, tongue, and jaw to build a case for whether a proper sleep study is needed. Catching these signs early is the first, most crucial step toward getting your health back.
Oral Appliance Therapy: A Comfortable and Effective Solution
If we see signs of a high risk for sleep apnea, we will refer you to a sleep specialist for a formal diagnosis. For many patients diagnosed with mild to moderate OSA, dentists can provide a highly effective, CPAP-free treatment called oral appliance therapy.
This therapy involves a custom-fitted device, similar to a mouthguard, that you wear while sleeping. It works by gently repositioning your lower jaw forward, which prevents the tongue and soft tissues from collapsing into your throat. This simple adjustment keeps your airway open all night. These devices are silent, portable, and easy to maintain, making them an excellent alternative for those who struggle with CPAP. To see if this could work for you, learning about sleep apnea treatment in Tempe is a great next step.
CPAP vs Oral Appliance Therapy: A Quick Comparison
Feature | CPAP Machine | Dental Oral Appliance |
|---|---|---|
How It Works | Delivers pressurized air through a mask to keep the airway open. | Gently repositions the lower jaw forward to prevent airway collapse. |
Best For | All levels of sleep apnea, especially severe cases. | Mild to moderate obstructive sleep apnea. |
Portability | Bulky and requires electricity, making travel a challenge. | Small, lightweight, and requires no power. Fits in your pocket. |
Noise Level | Machine produces a constant, low hum. Mask can have air leaks. | Completely silent during use. |
Comfort | Mask can be uncomfortable, restrictive, or cause skin irritation. | Custom-fit for comfort, but may cause initial jaw soreness. |
Maintenance | Requires regular cleaning of the mask, tubing, and water chamber. | Simple to clean with a toothbrush and cleaner. |
While CPAP is a powerful tool, oral appliances offer a life-changing solution for many who need a more comfortable and convenient option. Your next dental visit could be the first step toward finally solving your sleep problems.
Your Action Plan: From Symptoms to Solution
If you suspect sleep apnea is the reason for your persistent fatigue, it's time to take control. Moving from suspicion to a solution can feel overwhelming, but there is a clear path forward. Follow these steps to get your energy and your health back on track.
Step 1: Recognizing the Warning Signs
First, connect how you feel during the day with what might be happening at night. Many people dismiss these symptoms as stress or aging, but they often point to a treatable medical condition.
Ask yourself if any of these signs sound familiar:
Loud, disruptive snoring, especially if it includes pauses, choking, or gasping.
Persistent daytime sleepiness, no matter how much you sleep.
Waking up with a dry mouth, sore throat, or morning headaches.
Difficulty concentrating or feeling like your memory is failing.
Irritability, mood swings, or unexplainable feelings of depression.
If you're nodding along, it's time to take action.
Step 2: Starting the Conversation
Your primary care doctor or your dentist is the right person to talk to first. You don't need a self-diagnosis—just share your symptoms. Be direct: "I'm always tired, I snore loudly, and I'm concerned it could be sleep apnea." This simple statement can kickstart the diagnostic process.
Based on your symptoms and a physical exam, your provider can determine if a sleep study is necessary to get a definitive diagnosis.
This infographic shows how a routine dental visit can initiate this entire process.
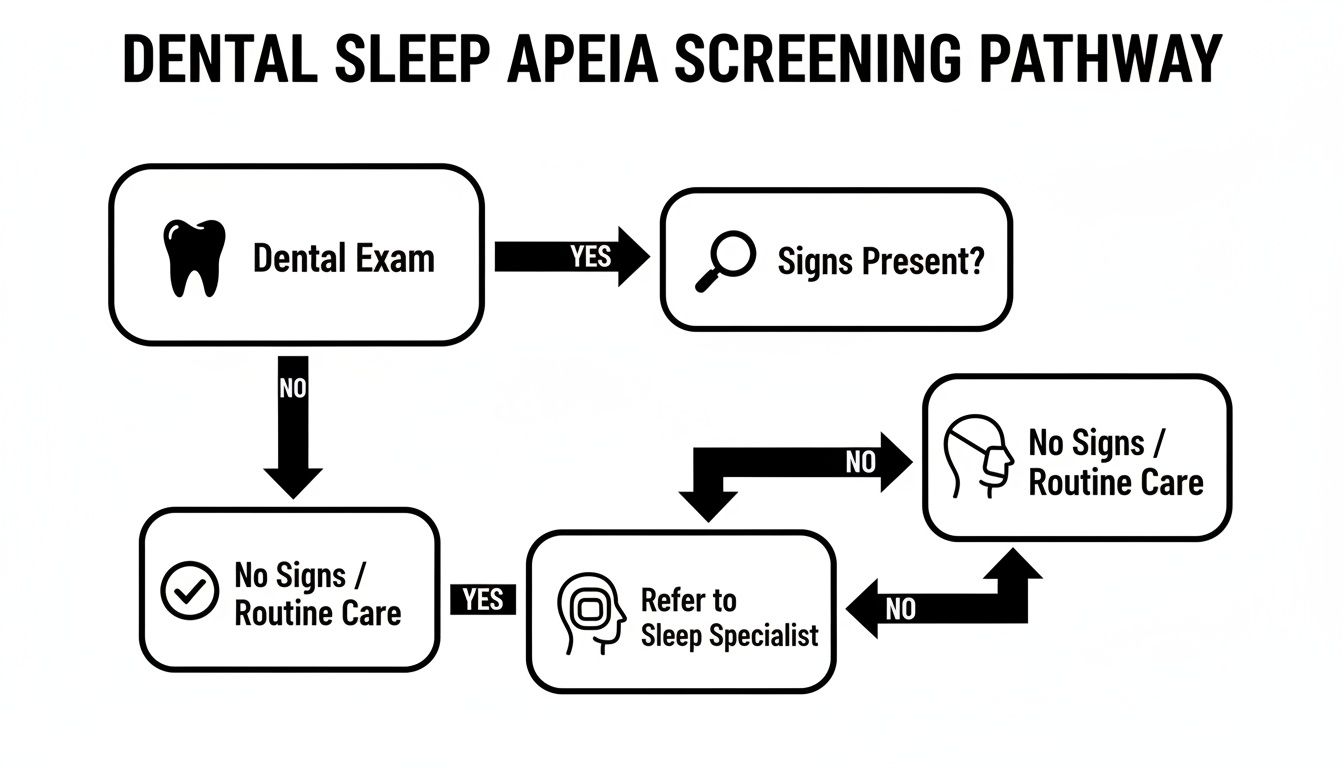
As you can see, a simple dental exam can be a powerful screening tool, spotting physical red flags that lead to a specialist referral and, ultimately, a solution.
Step 3: Undergoing a Sleep Study
A polysomnography, or sleep study, is the only way to definitively diagnose sleep apnea. This test measures your brain waves, heart rate, breathing patterns, and blood oxygen levels while you sleep. The results provide clear proof of whether you are experiencing breathing pauses and how severe they are.
You have two primary options:
In-Lab Study: You spend the night at a sleep center monitored by technicians. This is the most comprehensive option.
Home Sleep Apnea Test (HSAT): A convenient alternative for many, where you use a simple device to track your breathing and oxygen levels in your own bed.
Your doctor will recommend the appropriate test. The results will provide an Apnea-Hypopnea Index (AHI) score, which measures the severity of your condition and guides your treatment.
Step 4: Mapping Out Your Treatment Path
Once diagnosed, you and your healthcare team can create a personalized treatment plan. The goal is to keep your airway open so you can breathe continuously and get the restorative sleep you need.
A diagnosis isn't the end of the road—it's the start of the solution. Proper management can wipe out the health risks of sleep apnea and give you back the energy and vitality you've been missing.
Your plan will likely include one or more of these effective options:
CPAP (Continuous Positive Airway Pressure): A machine that delivers a steady stream of air through a mask to keep your airway open. It is the gold standard for moderate to severe cases.
Oral Appliance Therapy: A custom-fit dental device that moves your jaw forward to prevent airway collapse. It’s an excellent, comfortable alternative for mild to moderate OSA.
Lifestyle Modifications: Actions like managing your weight, reducing alcohol consumption, and quitting smoking can dramatically improve symptoms and are crucial for the success of any treatment.
In some cases, surgical options to correct anatomical issues may also be considered. No matter the path, the most important step is the first one: seeking help.
Common Questions About Sleep Apnea Causes
It’s normal to have questions as you learn about sleep apnea. Here are answers to some of the most common ones to provide clarity and guide your next steps.
Can I Have Sleep Apnea if I’m Not Overweight?
Yes, absolutely. While excess weight is a major risk factor, your anatomy is just as important. If you were born with a recessed jaw, large tonsils, or a narrow palate, your airway is naturally smaller. For you, the normal muscle relaxation during sleep can be enough to cause a collapse, regardless of your weight.
Does Snoring Always Mean I Have Sleep Apnea?
No. Simple snoring is just the sound of soft tissues vibrating in your throat and can be harmless. The snoring associated with sleep apnea is different. It's typically very loud and punctuated by pauses, followed by a gasp or choking sound as breathing restarts. If you notice this pattern, it is a strong signal that you should get evaluated.
Here's the key difference: While not every snorer has sleep apnea, almost everyone with obstructive sleep apnea snores. The pattern of the snoring is what tells the real story.
Is Sleep Apnea Something That Can Be Cured?
For some, yes. If sleep apnea is caused solely by excess weight, significant weight loss can sometimes resolve it. In children, removing enlarged tonsils and adenoids can be a permanent cure.
For most adults, however, sleep apnea is a chronic condition that requires ongoing management. The goal of treatment is to control it so effectively that it no longer poses a threat to your health. Therapies like CPAP and oral appliances can completely eliminate the symptoms and risks, allowing you to live a normal, healthy life.
How Can a Dentist Help With Snoring and Sleep Apnea?
A dentist trained in sleep medicine can be your first line of defense. During a routine exam, we can spot anatomical risk factors in your mouth that suggest an obstructed airway. If you are diagnosed with mild to moderate OSA by a sleep physician, we can create a custom-fitted oral appliance. This device works by holding your lower jaw in a forward position, which keeps your airway open all night. It is a comfortable, silent, and effective way to stop snoring and apnea events, helping you get the restorative sleep you've been missing.
At Beautiful Dentistry, we specialize in identifying the oral signs of sleep-disordered breathing and providing effective, patient-friendly solutions like custom oral appliance therapy. If you're tired of feeling tired, let us help you find the answers and the relief you deserve. Schedule your consultation at https://zdentist.com today.


Comments