How to Know If You Have Dry Socket: A Guide to Your Symptoms
- Caterina Rutter
- 5 hours ago
- 11 min read
After a tooth extraction, your main goal is a smooth recovery, but the risk of "dry socket" can be a major worry. This guide gives you actionable steps to identify the problem and know exactly what to do next.
A dry socket, clinically known as alveolar osteitis, is a common complication following a tooth removal. When a tooth is extracted, a blood clot must form in the empty socket. This clot is a natural bandage, protecting the underlying bone and nerves. A dry socket happens when this essential blood clot is dislodged, dissolves too early, or fails to form at all, leaving the sensitive area exposed.
What a Dry Socket Feels Like (And Who's Most at Risk)
The pain from a dry socket is not a typical toothache. It's a severe, deep, throbbing pain that often radiates from the extraction site toward your ear, eye, or temple on the same side of your face. You may also notice a bad taste or odor coming from your mouth.
If you gently look at the site in a mirror, instead of a dark, healing clot, you might see the whitish color of exposed jawbone. This exposure is what causes such intense pain—a level of discomfort that over-the-counter pain relievers usually can't manage.

This guide provides the practical information you need to identify a dry socket and take confident, decisive action.
Key Risk Factors You Should Know
While anyone can get a dry socket, certain factors significantly increase your risk. Being aware of these can help you take targeted preventive steps.
Here are the most common risk factors to watch for:
Tough Extractions: A difficult or surgical extraction, like removing impacted wisdom teeth, causes more trauma to the site, making it harder for the blood clot to remain stable.
Tobacco and Nicotine Use: Using tobacco is a major risk. The chemicals impair healing, while the act of inhaling can physically dislodge the clot from its socket.
Oral Contraceptives: The estrogen in some birth control pills can interfere with blood clotting, increasing the risk for some women.
Poor Aftercare: Not following your dentist's post-operative instructions can introduce bacteria or cause physical disruption that breaks down the essential blood clot.
It's a common myth that a dry socket is an infection. While it can lead to an infection, a dry socket itself is a healing complication caused by the physical loss of the protective blood clot.
Statistics confirm these risks. Dry socket occurs in about 3.2% of all extractions, but this number jumps to 12% for more complex surgical extractions. For simple removals, the rate is a much lower 1.7%. To understand the differences, you can get more details on wisdom teeth removal in Tempe.
Age is also a factor, with the highest incidence occurring in people between 18 and 33. You can explore the specific statistics on these risk factors for a more detailed look.
Decoding the Symptoms of a Dry Socket
After an extraction, some discomfort is normal. However, the pain from a dry socket is on a completely different level. Your most important action is to learn how to distinguish between normal healing and a true problem so you can get help quickly.
The defining symptom of a dry socket is a deep, throbbing pain that doesn't stay in one place. It radiates from the socket up toward your ear, eye, or temple. This is not the mild, localized soreness that improves each day. Instead, it's a severe pain that typically starts between the third and fifth day after your procedure—precisely when you should be feeling better.
What to Look For at the Extraction Site
You can often identify a problem with a simple visual check. In a well-lit mirror, carefully examine the extraction site. A healthy, healing socket should contain a dark, reddish blood clot.
Here are the visual cues of a dry socket to watch for:
An Empty Appearance: The socket may look hollow because the protective clot is gone.
Visible Bone: Instead of a dark clot, you might see the whitish or yellowish glint of the jawbone. This exposed bone is extremely sensitive.
Your only action here is to look—do not poke or probe the area. A quick, gentle visual inspection is all you need before calling your dentist.
The intense pain is a direct result of exposed bone and nerve endings being irritated by air, food, and fluids. This is why the pain feels so severe and why standard pain medication often provides little to no relief.
The Telltale Taste and Smell
Beyond the visual signs, a dry socket often produces other distinct symptoms. Many people report a persistent, foul taste in their mouth that gentle rinsing cannot eliminate.
This is frequently accompanied by bad breath (halitosis) that seems to originate directly from the extraction site. These symptoms are caused by food debris and bacteria accumulating in the unprotected socket. If you notice a foul taste or odor that wasn't present in the first couple of days, consider it a clear warning sign.
Recognizing these symptoms early is key. Research highlights that certain factors can increase your risk. For instance, females seem to have a slightly higher chance of developing dry socket; one study found that 66% of cases were in females, which might be linked to how oral contraceptives can affect blood clotting. The same study also pointed out a higher incidence in people aged 21-30. You can read more about these risk factors and demographic findings if you want to dig into the data.
Dry Socket Symptoms vs Normal Healing Discomfort
Use this checklist to determine if what you're experiencing is normal healing or a potential dry socket.
Symptom | Normal Healing Process | Potential Dry Socket |
|---|---|---|
Pain Level | Starts moderate, then steadily decreases over a few days. Can be managed with prescribed or OTC pain meds. | Starts as expected, but then suddenly intensifies around day 3-5. Often severe, throbbing, and radiating. |
Pain Location | Focused on the extraction site itself. May feel like a dull ache. | Radiates to the ear, eye, temple, or neck on the same side of the face. |
Appearance | A dark blood clot is visible inside the socket, which gradually gets smaller as gum tissue grows over it. | The socket looks empty, and you may see the whitish color of the underlying jawbone. |
Taste & Odor | You might have a slightly metallic or medicinal taste for the first day, but no foul odor. | A persistent bad taste and a noticeable foul odor (halitosis) coming from the socket. |
If your symptoms align with the "Potential Dry Socket" column, your next step is to contact your dentist or oral surgeon immediately. Do not attempt to wait it out.
The Post-Extraction Healing Timeline
Understanding the typical healing timeline is the best way to spot a problem early. A normal recovery follows a predictable pattern. By knowing these milestones, you can confidently differentiate between normal discomfort and the red flags of a dry socket.
On Day 1, your primary task is to protect the blood clot. You will experience some soreness and swelling, but it should be manageable with the pain medication your dentist recommended. The area will be tender, so avoid disturbing it.
By Days 2-3, you should notice a clear improvement. The initial soreness should be fading, and any swelling should be decreasing. This is a positive sign that your body is healing correctly and the blood clot is secure, protecting the sensitive bone and nerves.
The Critical Window for Dry Socket
The most important period to monitor is between Days 3 and 5 post-extraction. This is the peak window for a dry socket to develop. The key indicator is a sudden reversal of progress: instead of continuing to improve, your pain becomes significantly worse.
The actionable sign of a dry socket is pain that dramatically worsens after the second day. If you were feeling better and then the pain suddenly intensifies, that is your body's signal to call your dentist.
This timeline illustrates a normal recovery versus the onset of dry socket.
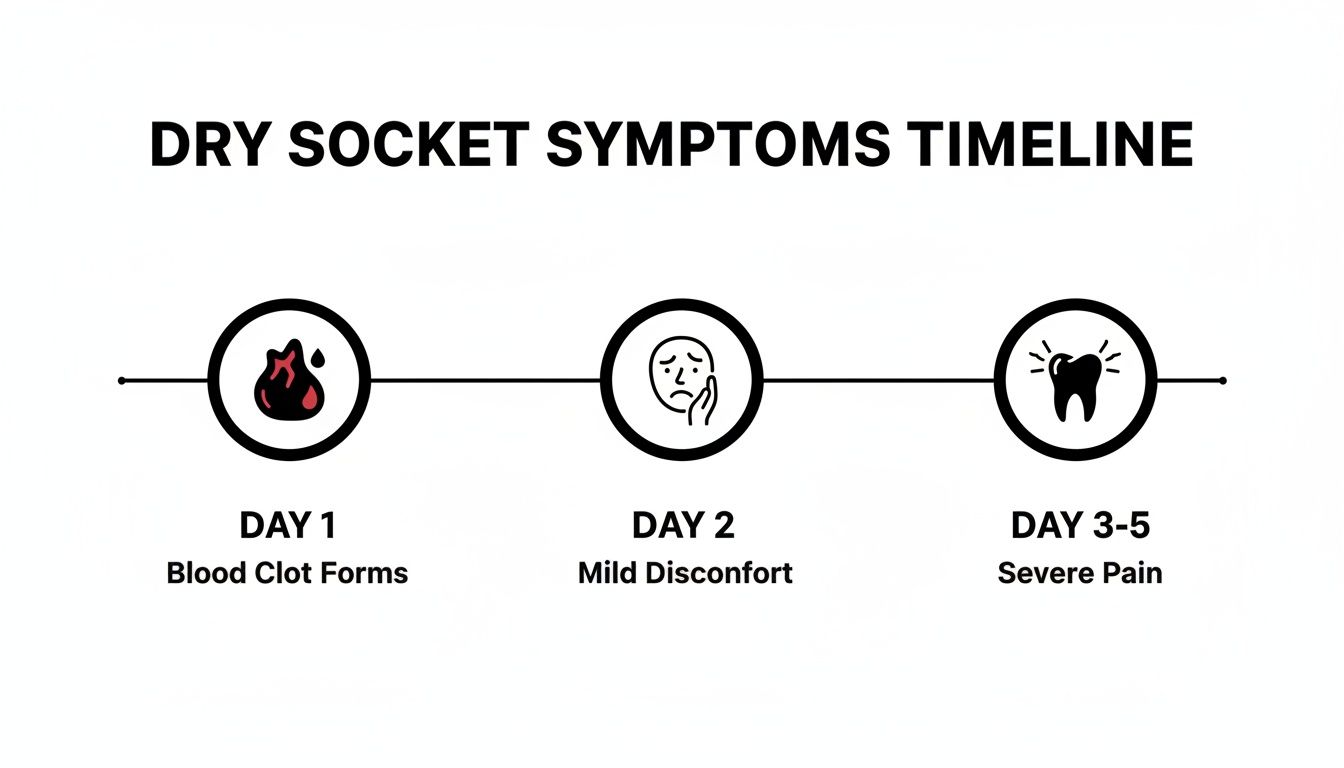
As you can see, some discomfort is expected. What is not normal is a sudden spike in severe, throbbing pain that radiates toward your ear several days into your recovery. That is the classic sign of a dry socket and your cue to take immediate action.
By comparing your experience to this timeline, you can assess your healing progress. A good recovery is a steady decrease in pain. A dry socket is a sudden U-turn back to severe pain.
For more proactive recovery strategies, review our fast recovery tips after a tooth extraction. Being prepared helps you heal properly and gives you the confidence to know exactly when you need to contact your dentist.
What to Do Right Now if You Suspect Dry Socket
If your symptoms point to a dry socket, it's time for clear, calm action. Your immediate goal is not to fix the problem yourself, but to manage the severe pain until you can see your dentist.
First, the most critical action is to do nothing to the socket itself. Resist the temptation to clean, poke, or pack anything into the area. Doing so will likely introduce bacteria, damage the exposed bone, and worsen the pain.
Immediate At-Home Measures for Pain Management
While you cannot cure a dry socket at home, you can take these specific steps to get temporary relief while you arrange professional care.
Gentle Saltwater Rinse: Mix half a teaspoon of salt into a glass of warm water. Do not swish vigorously. Instead, gently tilt your head from side to side, letting the solution flow over the site to dislodge any loose food particles.
Apply a Cold Pack: Wrap a cold pack or bag of frozen vegetables in a towel. Apply it to the outside of your cheek over the painful area for 15 minutes on, 15 minutes off. The cold helps numb the throbbing pain and reduce inflammation.
When Over-the-Counter Pain Relievers Don't Touch the Pain
It is reasonable to try an over-the-counter anti-inflammatory like ibuprofen. However, if standard pain medication provides little or no relief, consider this a confirmation that you are likely dealing with a dry socket.
Your number one action item is to call your dentist or oral surgeon immediately. When you call, be direct: report the severe, radiating pain that began several days after your extraction and state that standard pain medication is not working. This information will signal the urgency of your situation.
Waiting will only prolong your pain. Prompt professional treatment is the only effective solution. For a more detailed plan, see our actionable guide for handling a dry socket. Your dental team is prepared to handle this and will know exactly what to do.
How Your Dentist Will Treat a Dry Socket
If you suspect a dry socket, knowing the treatment process can help reduce anxiety. The procedure is straightforward, gentle, and focused on providing immediate pain relief.
First, your dentist will gently clean the extraction site. They will flush the socket with a sterile saline solution to remove any trapped food debris that is irritating the exposed bone and nerves. This step is crucial for preparing the area to heal correctly.
Placing a Medicated Dressing for Immediate Relief
After cleaning the socket, your dentist will perform the key step: placing a medicated dressing or paste directly into the socket. This dressing acts as a soothing, protective barrier.
These dressings are often infused with ingredients like eugenol (a component of clove oil), which has natural anesthetic and antiseptic properties. The medicated packing serves two immediate functions:
It physically shields the hypersensitive bone and nerve endings from air, food, and fluids.
It delivers soothing medication directly to the source of the pain, calming the irritated nerves.
The pain relief from this single step is typically dramatic and almost immediate. Most patients report their pain level dropping from severe to manageable within minutes of the dressing being placed.
Professional treatment is not just about pain relief; it's about restarting the healing process. The medicated dressing serves as a substitute for the lost blood clot, protecting the site so new tissue can begin to form.
Additional Steps for a Smooth Recovery
Your dentist may also prescribe antibiotics if there are signs of an infection. You will receive clear instructions for at-home care, which may include returning for a follow-up appointment in a day or two so your dentist can check your progress and replace the dressing if needed.
The classic sign that brings people in for this treatment is the visible absence of a blood clot a few days after the extraction, leaving the jawbone exposed. The pain is usually so severe that nothing you take at home even touches it. This complication is especially common after wisdom tooth removal, with some studies showing rates as high as 30%. Interestingly, the dentist's experience level seems to play a role; one study found that 57% of dry socket cases were associated with less experienced interns. You can read more about these clinical findings and risk factors if you're curious about the data.
Proactive Steps to Prevent Dry Socket

The most effective way to manage a dry socket is to prevent it from happening. The first few days after your tooth extraction are critical. Your only job is to protect the fragile blood clot that forms in the socket.
The primary threat to the blood clot is suction. Any action that creates negative pressure in your mouth can dislodge the clot. This is why your dentist will instruct you to avoid using straws and to stop all smoking or tobacco use.
Key Post-Operative Care Habits
Follow these actionable steps to significantly reduce your risk:
Avoid Forceful Spitting or Rinsing: Instead of spitting, allow liquids to passively fall from your mouth into the sink.
Stick to Soft Foods: For the first few days, eat only soft foods like yogurt, smoothies, mashed potatoes, and applesauce. Avoid anything hard, crunchy, or seedy that could become trapped in the socket.
Practice Gentle Oral Hygiene: Continue to brush your other teeth, but be extremely cautious and gentle near the extraction site.
If you know you are in a high-risk category—for example, if you smoke, have a history of dry socket, or take oral contraceptives—inform your dentist before the procedure. They can take extra preventive measures, such as using a special mouthwash or placing a protective dressing immediately after the extraction.
Following your dentist's post-operative instructions precisely is the most powerful action you can take to ensure a smooth, complication-free recovery.
Your Dry Socket Questions, Answered
Here are direct answers to the most common questions patients have after an extraction.
Can I Just Treat Dry Socket at Home?
No. While you can take steps to manage the pain temporarily, you cannot treat a dry socket yourself. You must see a dentist.
Professional treatment is required to properly clean the socket and place a medicated dressing. This dressing protects the exposed nerve and bone, provides immediate relief, and prevents infection. Attempting to pack the socket with cotton or any other material at home is dangerous and will worsen the problem.
How Long Is This Pain Going to Last?
If left untreated, the severe pain from a dry socket can last for a week or more.
However, with professional treatment, you should feel significant relief almost immediately after the dentist places the medicated dressing. This action gets the healing process back on track, and the worst of the pain typically subsides within 24 to 48 hours.
The purpose of the medicated dressing is to stop the pain cycle. It acts as a temporary replacement for the lost blood clot, allowing your body to resume the healing process without interference.
What if I Can See the Socket, but It Doesn't Hurt? Is That Still Dry Socket?
The defining symptom of a true dry socket is severe, worsening pain that is unresponsive to over-the-counter medication.
While it is technically possible to lose the clot without experiencing intense pain, this is extremely rare. Pain is the condition's hallmark. If you see an empty-looking socket but feel fine, it's still wise to have your dentist check it. However, without the signature escalating pain, it is likely not a true dry socket.
At Beautiful Dentistry, we want your recovery to be as smooth and comfortable as possible. If you're in the Tempe area and something about your healing process just doesn't feel right, please don't wait and wonder. Our experienced team is here to give you the answers and gentle care you need. You can learn more about us at https://zdentist.com.


Comments